Alapadatok
Év, oldalszám:2017, 5 oldal
Nyelv:angol
Letöltések száma:2
Feltöltve:2022. december 02.
Méret:1 MB
Intézmény:
-
Megjegyzés:
Csatolmány:-
Letöltés PDF-ben:Kérlek jelentkezz be!
Értékelések
Nincs még értékelés. Legyél Te az első!Tartalmi kivonat
Clinical REVIEW Rosacea - An overview on the diagnosis and assessment Paula Oliver Abstract This article provides an overview of the assessment, diagnosis and treatment options for rosacea Citation: Oliver P (2017) Rosacea – An overview on the diagnosis and assessment. Dermatological Nursing 17(2):10-14 Rosacea is a common chronic inflammatory disorder of the skin predominantly affecting the central face. It is characterised by frequent flushing, persistent erythema, telangiectasia and interspersed with episodes of inflammation during which patients experience tissue swelling with papules and pustules. Patients may also experience ocular lesions and rhinophymas (excess growth of tissue of the nose) and cutaneous sensations often include stinging and burning. It typically appears between the ages of 30-60.1 Phymatous rosacea can also affect other areas on the face such as the chin (gnathophymas), ears (otophyma), forehead (mentophyma) or the eyelids (blepharophyma).
Characteristically, rosacea is a condition of the white population and it is three times more common in women than men.2 Paula Oliver RGN BSc(Hons) MSc INP holds an honorary clinical role at Sussex Community Dermatology Service and Brighton and Sussex University Hospitals NHS Trust. Nurse Consultant/Team Leader for Galderma (UK) Ltd 10 The word rosacea is derived from the Latin adjective meaning like roses.3 The term acne rosacea and adult acne are misleading and obsolete, acne and rosacea are separate disease processes, even though they may co-exist at times. It is therefore important to establish the correct disease diagnosis to ensure that an appropriate treatment plan may be implemented. The psychosocial impact of living with rosacea can adversely impact an individual’s well-being, and that level of psychological burden should influence treatment decisions. In addition, there is also a psychosocial impact associated with rosacea treatments. Patients can become disheartened as
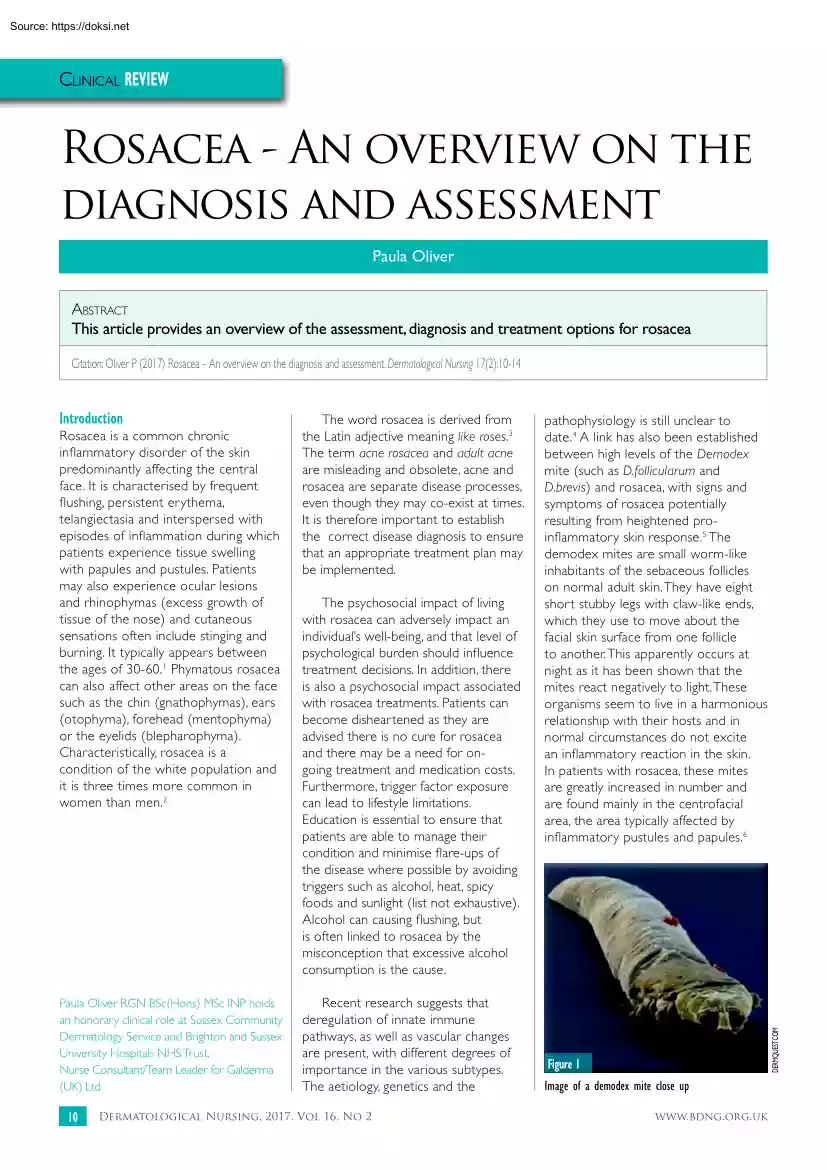
they are advised there is no cure for rosacea and there may be a need for ongoing treatment and medication costs. Furthermore, trigger factor exposure can lead to lifestyle limitations. Education is essential to ensure that patients are able to manage their condition and minimise flare-ups of the disease where possible by avoiding triggers such as alcohol, heat, spicy foods and sunlight (list not exhaustive). Alcohol can causing flushing, but is often linked to rosacea by the misconception that excessive alcohol consumption is the cause. Recent research suggests that deregulation of innate immune pathways, as well as vascular changes are present, with different degrees of importance in the various subtypes. The aetiology, genetics and the Dermatological Nursing, 2017, Vol 16, No 2 pathophysiology is still unclear to date.4 A link has also been established between high levels of the Demodex mite (such as D.follicularum and D.brevis) and rosacea, with signs and symptoms of rosacea
potentially resulting from heightened proinflammatory skin response.5 The demodex mites are small worm-like inhabitants of the sebaceous follicles on normal adult skin. They have eight short stubby legs with claw-like ends, which they use to move about the facial skin surface from one follicle to another. This apparently occurs at night as it has been shown that the mites react negatively to light. These organisms seem to live in a harmonious relationship with their hosts and in normal circumstances do not excite an inflammatory reaction in the skin. In patients with rosacea, these mites are greatly increased in number and are found mainly in the centrofacial area, the area typically affected by inflammatory pustules and papules.6 DermQuest.com Introduction Figure 1 Image of a demodex mite close up www.bdngorguk Clinical REVIEW Consensus recommendations in 2002 suggested that rosacea was classified into four subtypes based on the clinical presentation, as follows: 8
Erythematotelangiectatic rosacea (ETTR); 8 Papulopustular (PPR); 8 Phymatous rosacea (PYR); and 8 Ocular rosacea (OR). Rosacea features can span multiple subtypes and progress between subtypes. Therefore, their clinical presentation may be more accurately defined by the term phenotype (individual features), which describes an individual’s observable characteristics that can be influence by genetic or environmental factors. Subtype classification may not fully cover the range of clinical presentations and is likely to confuse severity assessment, whereas a phenotype-based approach could improve patient outcomes by addressing an individual patient’s clinical presentation and their concerns. Tan et al suggests that adopting a phenotype led approach will address rosacea and its treatments in a way that is more consistent with the individual’s experience.8 The disease is unpredictable and can vary from week to week for patients. This can affect the patient’s quality of life. In
addition to the physical impact, it is well documented that patients report significant psychological distress owing to the sometimes dramatic changeable nature of the signs and symptoms. The National Rosacea Society (NRS) conducted a survey of 1,675 patients, of which 90% of respondents said the effects of the disease on their personal appearance had lowered their self-esteem and self-confidence; 88% reported embarrassment; and others noted feelings of frustration (76%), anxiety and helplessness (54%), depressions (43%), anger (34%), and isolation (32%) www.bdngorguk Figure 2 Erythematotelangiectatic rosacea (ETTR) Figure 3 Papulopustular (PPR)I DermQuest.com However patients often present with a varied range of symptoms that overlap these sub-types.7 As an example, patients may present with papulopustular rosacea and also persistent erythema, and even if the PPR is treated successfully the erythema either transient or fixed may still remain. Figure 4 Phymatous rosacea (PYR)
Dermatological Nursing, 2017, Vol 16, No 2 11 Clinical REVIEW Primary features The presence of one or more of the following signs with central face distribution is suggestive of rosacea, although patients may have more than one of these features: 8 Flushing 8 Persistent erythema of the facial skin 8 Dome-shaped papules with or without pustules and nodule may also be present 8 Telangiectasia. Theses often appear with one or more of the primary features but also may appear independently: 8 Burning or stinging 8 Raised plaques 8 Dry appearance rough and scaling 8 Oedema 8 Ocular signs that may include burning , itching, hyperemia, inflammation, styes, chalazia 8 Peripheral location 8 Phymatous changes. Rosacea can resemble other dermatological disorders, including acne and systemic lupus erythematosus Differential diagnosis ETTR is characterised by centrofacial erythema, a tendency to flush frequently and typically prominent facial telangiectasias. PPR is usually diagnosed on the
clinical appearance of erythema, papules and pustules in a centrofacial distribution. In PYR, a range of phymatous changes may be seen in patients with rosacea, however rhinophyma is the most common and mainly occurs in males. Finally OR is common and is often overlooked by the patients and the healthcare professional, symptoms are usually mild and serious consequences of OR are rare. Rosacea can resemble other dermatological disorders, including acne and systemic lupus erythematosus (SLE). Acne is more 12 DermQuest.com Secondary features Figure 5 Ocular rosacea (OR) commonly seen in teenage years, while rosacea occurs most often between 30-60 years of age. Also, in acne, unlike rosacea, open comedones (blackheads) are generally present, and papules and pustules on extra facial locations such as trunk and upper arms are common. While SLE and rosacea share some manifestations, including facial erythema, sensitivity to ultra violet light and tends to affect more females than males,
clinicians have often used serology screening or histopathology to confirm the diagnosis of SLE. Triggers Sign and symptoms of rosacea can be Sun Emotional stress Hot weather Wind Heavy exercise Alcohol Hot baths Cold weather Spicy foods Humidity Certain skin care products Indoor heat Heated beverages Certain cosmetics triggered by environmental factors, including sun exposure, temperature changes, stress and spicy foods to name a few. However, affected rosacea skin exhibits increased sensitivity to these triggers and patients need to try and identify their own individual triggers that exacerbates their condition. Besides trigger avoidance, the most common treatment approaches to rosacea are pharmacological in nature. Emollients and sunscreen are recommended for all rosacea patients to stabilise the skin’s barrier dysfunction and to help prevent 81% 79% 75% 57% 56% 52% 51% 46% 45% 44% 41% 41% 36% 27% Figure 6 Known triggers: National Rosacea Society Results based on a survey of
1,066 rosacea patients trigger for rosacea http://www.rosaceaorg/patients/materials/triggersgraphphp Website last accessed: March 2017 Dermatological Nursing, 2017, Vol 16, No 2 www.bdngorguk Clinical REVIEW photo-aggravation. Patients may need to explore a range of products to find one that will suit their skin as moisturisers, make-up and sunscreen can potentially irritant sensitive skin. Identifying trigger factors is an individual process and what may cause a skin reaction in one patient may not in another. A rosacea diary could include a daily checklist of the most common factors that trigger rosacea flare- ups in patients. Patients can complete a daily log and look for items that seem to coincide with any rosacea flare. Management of symptoms and treatment options Patients should be provided with an information leaflet to inform them on how to minimise their triggers, which may aggravate their condition, and also how to care for their skin with a simple skin cleansing and
moisturising regime. The Primary Care Dermatology Society (PCDS)9 has recently reviewed and published rosacea management guidelines that are available at www.pcdsorg Flushing/erythema and telangiectasia Flushing of the face is caused by facial vasodilation leading to increased cutaneous blood flow.6 Causes of flushing include rosacea, alcohol, spices, some drugs including calcium channel blockers, and neurological disorders. For many patients this can be a prominent cutaneous symptom and has a profound impact on a patient’s quality of life. Transient flushing on the central aspects of the face (which can last for minutes) may be helped in the short term by a nonselective cardiovascular beta-blocker such as propranolol 40mg BD or clonidine 50mcg BD. If the erythema is persistent and causing psychological distress, Brimonidine Tartrate topical gel 0.33%, an alpha adrenergic agonist, is indicated for the topical treatment of persistent facial erythema in adults aged 18 years or over.
This needs to be applied thinly once a day and its mode of action is to constrict the facial blood vessels causing a temporary reduction in the erythema. www.bdngorguk Patients need to be instructed how to apply the gel evenly to achieve a good outcome. Laser therapy using a pulsed dye laser is also an option for patient that can self-fund. Pulsed dye laser treatment targets redness of rosacea by delivering a long pulse of energy to the affected areas. It will often entail several treatment sessions over a period of weeks. This can be very effective and improve the cosmetic appearance for patients but rarely will be funded on the NHS. Cosmetic camouflage is also an option and patients can explore more about this via the Changing Faces website.10 Identifying trigger factors is an individual process and what may cause a skin reaction in one patient may not in another Cosmetic camouflage can be used to cover the skin, and over the years has helped numerous patients with a wide variety
of skin conditions. Trained skin camouflage practitioners will find the best colour match for each person skin tone and then teach them how to self-apply the specialist cover products. The products are fully waterproof and are available on prescription from general practitioners; the products are listed in the British National Formulary (BNF) in the borderline substance’s section. Papules, pustules and nodules In inflammatory PPR patients should be advised that while a chronic condition that cannot be cured it can be very well controlled by using anti-inflammatory treatments and if required in the long term nonantibiotic therapies are preferable to reduce increasing antibiotic resistance. If patients symptoms are mild to moderate topical therapies such as ivermectin 10mg/g cream provides a newer antibiotic-free treatment option, is applied once a day to facial skin and is tolerated well. Its mode of action is anti-inflammatory and anti-parasitic, thereby reducing inflammation and
inhibiting the demodex mite. Metronidazole 0.75% gel or cream historically has been used for PPR and also azealic acid 15% cream these need applying twice daily both have an anti-microbial mode of action. In more severe cases, or if topical treatments fail, an antibiotic may be necessary using a tetracycline e.g oxytetracycline 500mg BD, lymecycline 408mg OD or a low dose doxycycline 40mg. The low dose doxycyline 40mg delivers an anti-inflammatory dose rather than an anti-microbial dose to the patient. Erythromycin 500mg BD is also an alternative. As rosacea is a chronic inflammatory condition it is not ideal to continue on systemic antibiotics in the long term so treatment is usually recommended for a minimum of three months then to reduce the dose. For severe disease that responds poorly to treatment, referral to a dermatologist should be considered for assessment and a low dose of isotretinoin may be potentially recommended. Rhinophymas Patients with rhinophymas respond very well to
CO2 laser or surgical shave excision. Both of these treatments are designed to remove the excess of affected tissue. Ocular symptoms Patients presenting with ocular symptoms can experience ‘gritty’ eyes, conjunctivitis, blepharitis and chalazion, which are cysts on the eyelids. It is thought that 50% of patients with diagnosed rosacea have ocular involvement. Educating patients on eyelid hygiene is important. Eyelids can be cleaned using cotton wool soaked in boiled cooled water. Artificial tears can help the ‘gritty’ sensation experienced by some patients. Systemic tetracyclines are the most effective treatment for ocular rosacea. Systemic retinoids such as isotretinion are generally avoided in patients with severe ocular problems as they can worsen symptoms. If severe symptoms Dermatological Nursing, 2017, Vol 16, No 2 13 Clinical REVIEW persist a referral to an ophthalmologist for further management may be necessary. Reducing antibiotic therapies The World Health
Organization (WHO) has spoken about the evolving threat of antimicrobial resistance and has called for action globally. This year, World Antibiotic Awareness Week will be held from 13-19th November 2017 and all healthcare professionals are urged to join the campaign. Roughly 8% of all antibiotics prescribed in the United Kingdom are thought to be for a dermatological indication.11 Considering that rosacea is a chronic inflammatory condition, clinicians need to consider the appropriateness of the long term use of both topical and systemic antibiotics and explore alternative non-antibiotics treatment when possible. The Psychological impact of Rosacea “.there was a summoner with us at that inn, his face on fire like a cherubin, for he had carbuncles.no quicksilver, lead ointment, tartar creams, no brimstone, no boric, so it seems, could make a salve that had the power to bite, clean up or cure his whelks or knobberly white or purge the pimples sitting on his cheeks. Chaucer,
(Canterbury Tales) The psychological impact of living with a skin condition is well documented.12 Psychological difficulties for skin patients include increased levels of anxiety and depression, concerns with body image, low self-esteem and concerns with social interactions. A survey was conducted to explore GP’s provision of psychological care to patients with rosacea and psoriasis and they found that the most commonly reported symptoms for 14 both the conditions were concern over the appearance with feelings of embarrassment.13 Roughly 8% of all antibiotics prescribed in the United Kingdom are thought to be for a dermatological indication Patients also described their concerns by physical symptoms including erythema, papules and pustules and the facial redness for rosacea. Although in the author’s experience, controversially on occasions HCPs have suggested that these symptoms are of cosmetic concern and don’t require interventions. The survey provided further evidence that
the psychological needs of these patients are not being met and the important role for dermatology nurses acting as the patients advocate and performing psychological assessment and also ensuring that other HCPs are adhering to best practice. Conclusion Rosacea is a chronic inflammatory skin condition that is clearly visible, but its cause is often unknown and it is misunderstood by the general public. The visible appearance is often distressing and the relapsing and remitting nature of the condition may have a negative impact on a patient’s quality of life. Nurses can play an important role in educating and supporting patients about the skin diagnosis and its management. As well as the psychological support, nurses can discuss lifestyle changes and triggers that may reduce the flare-up frequency. In the future, healthcare professionals may be treating patients on the individual clinical presentation and target the treatments accordingly, rather than attempting to treat each subtype
as discussed in this article. DN Conflict of interest Paula is also a Nurse Consultant/ Team Leader for Galderma (UK) Ltd. This article is not endorsed by Galderma (UK) Ltd. Dermatological Nursing, 2017, Vol 16, No 2 References 1. Wolf JE Rosacea: Diagnosis and management of a complex and significant disorder. Consultant 2016, 56(10) 901-905 2. Stollery N Managing patients with rosacea. MIMS Dermatology 2017, 13(1) 36-37 3. Plegwin G Kligman A Acne and Rosacea. 3rd Completely revised and enlarged edition. Springer New York 2000 p456 4. Holmes A D Steinhoff M Integrative concepts of rosacea pathophysiology, clinical presentation and new therapeutics. Experimental Dermatology 2016, 1-9 5. Steinhoff M, Vocanson M, Voegel J, Hacini-Rachinel F, Schafer G. Topical Ivermectin 10mg/g and oral Doxycycline 40mg Modified-release: Current evidence on the complementary use of anti-inflammatory Rosacea treatments. Adv Ther 2016, 33 1481-1501 6. Powell FC Rosacea Diagnosis and management. Informa
Healthcare 2009 Chapter 5 p69 7. Baldwin HE Diagnosis and treatment of Rosacea: state of the art. J Drugs and Dermatol 2012, 11(6) 725-30 8. Tan J, Almeida LMC, Bewley, A et al Updating the diagnosis, classification and assessment of roscea: recommendations from the global ROSacea COsensus (ROSCO) panel. British Journal of Dermatology 2017, 176 431-438 9. Primary Care Dermatology Society (PCDS) www.pcdsorguk [last accessed April 2017] 10. Changing Faces Charity www changingfaces.orguk [last accessed April 2017] 11. Walsh TR, Dreno B Antibiotic resistance in acne, an increasing topical and oral threat: a systemic review. The Lancet Infectious Diseases 2016, 16(3) 12. Moustafa et al The psychological impact of Rosacea and the influence of current management options. J Am Acad 2014, 71(5)973-80 13. Krasuska M, Millings A, Lavda A, Thompson A. Psychological needs and availability of support for people with Rosacea and Psoriasis findings from a GP survey. Dermatological Nursing 2016 15(2)
48-49 www.bdngorguk
Characteristically, rosacea is a condition of the white population and it is three times more common in women than men.2 Paula Oliver RGN BSc(Hons) MSc INP holds an honorary clinical role at Sussex Community Dermatology Service and Brighton and Sussex University Hospitals NHS Trust. Nurse Consultant/Team Leader for Galderma (UK) Ltd 10 The word rosacea is derived from the Latin adjective meaning like roses.3 The term acne rosacea and adult acne are misleading and obsolete, acne and rosacea are separate disease processes, even though they may co-exist at times. It is therefore important to establish the correct disease diagnosis to ensure that an appropriate treatment plan may be implemented. The psychosocial impact of living with rosacea can adversely impact an individual’s well-being, and that level of psychological burden should influence treatment decisions. In addition, there is also a psychosocial impact associated with rosacea treatments. Patients can become disheartened as
they are advised there is no cure for rosacea and there may be a need for ongoing treatment and medication costs. Furthermore, trigger factor exposure can lead to lifestyle limitations. Education is essential to ensure that patients are able to manage their condition and minimise flare-ups of the disease where possible by avoiding triggers such as alcohol, heat, spicy foods and sunlight (list not exhaustive). Alcohol can causing flushing, but is often linked to rosacea by the misconception that excessive alcohol consumption is the cause. Recent research suggests that deregulation of innate immune pathways, as well as vascular changes are present, with different degrees of importance in the various subtypes. The aetiology, genetics and the Dermatological Nursing, 2017, Vol 16, No 2 pathophysiology is still unclear to date.4 A link has also been established between high levels of the Demodex mite (such as D.follicularum and D.brevis) and rosacea, with signs and symptoms of rosacea
potentially resulting from heightened proinflammatory skin response.5 The demodex mites are small worm-like inhabitants of the sebaceous follicles on normal adult skin. They have eight short stubby legs with claw-like ends, which they use to move about the facial skin surface from one follicle to another. This apparently occurs at night as it has been shown that the mites react negatively to light. These organisms seem to live in a harmonious relationship with their hosts and in normal circumstances do not excite an inflammatory reaction in the skin. In patients with rosacea, these mites are greatly increased in number and are found mainly in the centrofacial area, the area typically affected by inflammatory pustules and papules.6 DermQuest.com Introduction Figure 1 Image of a demodex mite close up www.bdngorguk Clinical REVIEW Consensus recommendations in 2002 suggested that rosacea was classified into four subtypes based on the clinical presentation, as follows: 8
Erythematotelangiectatic rosacea (ETTR); 8 Papulopustular (PPR); 8 Phymatous rosacea (PYR); and 8 Ocular rosacea (OR). Rosacea features can span multiple subtypes and progress between subtypes. Therefore, their clinical presentation may be more accurately defined by the term phenotype (individual features), which describes an individual’s observable characteristics that can be influence by genetic or environmental factors. Subtype classification may not fully cover the range of clinical presentations and is likely to confuse severity assessment, whereas a phenotype-based approach could improve patient outcomes by addressing an individual patient’s clinical presentation and their concerns. Tan et al suggests that adopting a phenotype led approach will address rosacea and its treatments in a way that is more consistent with the individual’s experience.8 The disease is unpredictable and can vary from week to week for patients. This can affect the patient’s quality of life. In
addition to the physical impact, it is well documented that patients report significant psychological distress owing to the sometimes dramatic changeable nature of the signs and symptoms. The National Rosacea Society (NRS) conducted a survey of 1,675 patients, of which 90% of respondents said the effects of the disease on their personal appearance had lowered their self-esteem and self-confidence; 88% reported embarrassment; and others noted feelings of frustration (76%), anxiety and helplessness (54%), depressions (43%), anger (34%), and isolation (32%) www.bdngorguk Figure 2 Erythematotelangiectatic rosacea (ETTR) Figure 3 Papulopustular (PPR)I DermQuest.com However patients often present with a varied range of symptoms that overlap these sub-types.7 As an example, patients may present with papulopustular rosacea and also persistent erythema, and even if the PPR is treated successfully the erythema either transient or fixed may still remain. Figure 4 Phymatous rosacea (PYR)
Dermatological Nursing, 2017, Vol 16, No 2 11 Clinical REVIEW Primary features The presence of one or more of the following signs with central face distribution is suggestive of rosacea, although patients may have more than one of these features: 8 Flushing 8 Persistent erythema of the facial skin 8 Dome-shaped papules with or without pustules and nodule may also be present 8 Telangiectasia. Theses often appear with one or more of the primary features but also may appear independently: 8 Burning or stinging 8 Raised plaques 8 Dry appearance rough and scaling 8 Oedema 8 Ocular signs that may include burning , itching, hyperemia, inflammation, styes, chalazia 8 Peripheral location 8 Phymatous changes. Rosacea can resemble other dermatological disorders, including acne and systemic lupus erythematosus Differential diagnosis ETTR is characterised by centrofacial erythema, a tendency to flush frequently and typically prominent facial telangiectasias. PPR is usually diagnosed on the
clinical appearance of erythema, papules and pustules in a centrofacial distribution. In PYR, a range of phymatous changes may be seen in patients with rosacea, however rhinophyma is the most common and mainly occurs in males. Finally OR is common and is often overlooked by the patients and the healthcare professional, symptoms are usually mild and serious consequences of OR are rare. Rosacea can resemble other dermatological disorders, including acne and systemic lupus erythematosus (SLE). Acne is more 12 DermQuest.com Secondary features Figure 5 Ocular rosacea (OR) commonly seen in teenage years, while rosacea occurs most often between 30-60 years of age. Also, in acne, unlike rosacea, open comedones (blackheads) are generally present, and papules and pustules on extra facial locations such as trunk and upper arms are common. While SLE and rosacea share some manifestations, including facial erythema, sensitivity to ultra violet light and tends to affect more females than males,
clinicians have often used serology screening or histopathology to confirm the diagnosis of SLE. Triggers Sign and symptoms of rosacea can be Sun Emotional stress Hot weather Wind Heavy exercise Alcohol Hot baths Cold weather Spicy foods Humidity Certain skin care products Indoor heat Heated beverages Certain cosmetics triggered by environmental factors, including sun exposure, temperature changes, stress and spicy foods to name a few. However, affected rosacea skin exhibits increased sensitivity to these triggers and patients need to try and identify their own individual triggers that exacerbates their condition. Besides trigger avoidance, the most common treatment approaches to rosacea are pharmacological in nature. Emollients and sunscreen are recommended for all rosacea patients to stabilise the skin’s barrier dysfunction and to help prevent 81% 79% 75% 57% 56% 52% 51% 46% 45% 44% 41% 41% 36% 27% Figure 6 Known triggers: National Rosacea Society Results based on a survey of
1,066 rosacea patients trigger for rosacea http://www.rosaceaorg/patients/materials/triggersgraphphp Website last accessed: March 2017 Dermatological Nursing, 2017, Vol 16, No 2 www.bdngorguk Clinical REVIEW photo-aggravation. Patients may need to explore a range of products to find one that will suit their skin as moisturisers, make-up and sunscreen can potentially irritant sensitive skin. Identifying trigger factors is an individual process and what may cause a skin reaction in one patient may not in another. A rosacea diary could include a daily checklist of the most common factors that trigger rosacea flare- ups in patients. Patients can complete a daily log and look for items that seem to coincide with any rosacea flare. Management of symptoms and treatment options Patients should be provided with an information leaflet to inform them on how to minimise their triggers, which may aggravate their condition, and also how to care for their skin with a simple skin cleansing and
moisturising regime. The Primary Care Dermatology Society (PCDS)9 has recently reviewed and published rosacea management guidelines that are available at www.pcdsorg Flushing/erythema and telangiectasia Flushing of the face is caused by facial vasodilation leading to increased cutaneous blood flow.6 Causes of flushing include rosacea, alcohol, spices, some drugs including calcium channel blockers, and neurological disorders. For many patients this can be a prominent cutaneous symptom and has a profound impact on a patient’s quality of life. Transient flushing on the central aspects of the face (which can last for minutes) may be helped in the short term by a nonselective cardiovascular beta-blocker such as propranolol 40mg BD or clonidine 50mcg BD. If the erythema is persistent and causing psychological distress, Brimonidine Tartrate topical gel 0.33%, an alpha adrenergic agonist, is indicated for the topical treatment of persistent facial erythema in adults aged 18 years or over.
This needs to be applied thinly once a day and its mode of action is to constrict the facial blood vessels causing a temporary reduction in the erythema. www.bdngorguk Patients need to be instructed how to apply the gel evenly to achieve a good outcome. Laser therapy using a pulsed dye laser is also an option for patient that can self-fund. Pulsed dye laser treatment targets redness of rosacea by delivering a long pulse of energy to the affected areas. It will often entail several treatment sessions over a period of weeks. This can be very effective and improve the cosmetic appearance for patients but rarely will be funded on the NHS. Cosmetic camouflage is also an option and patients can explore more about this via the Changing Faces website.10 Identifying trigger factors is an individual process and what may cause a skin reaction in one patient may not in another Cosmetic camouflage can be used to cover the skin, and over the years has helped numerous patients with a wide variety
of skin conditions. Trained skin camouflage practitioners will find the best colour match for each person skin tone and then teach them how to self-apply the specialist cover products. The products are fully waterproof and are available on prescription from general practitioners; the products are listed in the British National Formulary (BNF) in the borderline substance’s section. Papules, pustules and nodules In inflammatory PPR patients should be advised that while a chronic condition that cannot be cured it can be very well controlled by using anti-inflammatory treatments and if required in the long term nonantibiotic therapies are preferable to reduce increasing antibiotic resistance. If patients symptoms are mild to moderate topical therapies such as ivermectin 10mg/g cream provides a newer antibiotic-free treatment option, is applied once a day to facial skin and is tolerated well. Its mode of action is anti-inflammatory and anti-parasitic, thereby reducing inflammation and
inhibiting the demodex mite. Metronidazole 0.75% gel or cream historically has been used for PPR and also azealic acid 15% cream these need applying twice daily both have an anti-microbial mode of action. In more severe cases, or if topical treatments fail, an antibiotic may be necessary using a tetracycline e.g oxytetracycline 500mg BD, lymecycline 408mg OD or a low dose doxycycline 40mg. The low dose doxycyline 40mg delivers an anti-inflammatory dose rather than an anti-microbial dose to the patient. Erythromycin 500mg BD is also an alternative. As rosacea is a chronic inflammatory condition it is not ideal to continue on systemic antibiotics in the long term so treatment is usually recommended for a minimum of three months then to reduce the dose. For severe disease that responds poorly to treatment, referral to a dermatologist should be considered for assessment and a low dose of isotretinoin may be potentially recommended. Rhinophymas Patients with rhinophymas respond very well to
CO2 laser or surgical shave excision. Both of these treatments are designed to remove the excess of affected tissue. Ocular symptoms Patients presenting with ocular symptoms can experience ‘gritty’ eyes, conjunctivitis, blepharitis and chalazion, which are cysts on the eyelids. It is thought that 50% of patients with diagnosed rosacea have ocular involvement. Educating patients on eyelid hygiene is important. Eyelids can be cleaned using cotton wool soaked in boiled cooled water. Artificial tears can help the ‘gritty’ sensation experienced by some patients. Systemic tetracyclines are the most effective treatment for ocular rosacea. Systemic retinoids such as isotretinion are generally avoided in patients with severe ocular problems as they can worsen symptoms. If severe symptoms Dermatological Nursing, 2017, Vol 16, No 2 13 Clinical REVIEW persist a referral to an ophthalmologist for further management may be necessary. Reducing antibiotic therapies The World Health
Organization (WHO) has spoken about the evolving threat of antimicrobial resistance and has called for action globally. This year, World Antibiotic Awareness Week will be held from 13-19th November 2017 and all healthcare professionals are urged to join the campaign. Roughly 8% of all antibiotics prescribed in the United Kingdom are thought to be for a dermatological indication.11 Considering that rosacea is a chronic inflammatory condition, clinicians need to consider the appropriateness of the long term use of both topical and systemic antibiotics and explore alternative non-antibiotics treatment when possible. The Psychological impact of Rosacea “.there was a summoner with us at that inn, his face on fire like a cherubin, for he had carbuncles.no quicksilver, lead ointment, tartar creams, no brimstone, no boric, so it seems, could make a salve that had the power to bite, clean up or cure his whelks or knobberly white or purge the pimples sitting on his cheeks. Chaucer,
(Canterbury Tales) The psychological impact of living with a skin condition is well documented.12 Psychological difficulties for skin patients include increased levels of anxiety and depression, concerns with body image, low self-esteem and concerns with social interactions. A survey was conducted to explore GP’s provision of psychological care to patients with rosacea and psoriasis and they found that the most commonly reported symptoms for 14 both the conditions were concern over the appearance with feelings of embarrassment.13 Roughly 8% of all antibiotics prescribed in the United Kingdom are thought to be for a dermatological indication Patients also described their concerns by physical symptoms including erythema, papules and pustules and the facial redness for rosacea. Although in the author’s experience, controversially on occasions HCPs have suggested that these symptoms are of cosmetic concern and don’t require interventions. The survey provided further evidence that
the psychological needs of these patients are not being met and the important role for dermatology nurses acting as the patients advocate and performing psychological assessment and also ensuring that other HCPs are adhering to best practice. Conclusion Rosacea is a chronic inflammatory skin condition that is clearly visible, but its cause is often unknown and it is misunderstood by the general public. The visible appearance is often distressing and the relapsing and remitting nature of the condition may have a negative impact on a patient’s quality of life. Nurses can play an important role in educating and supporting patients about the skin diagnosis and its management. As well as the psychological support, nurses can discuss lifestyle changes and triggers that may reduce the flare-up frequency. In the future, healthcare professionals may be treating patients on the individual clinical presentation and target the treatments accordingly, rather than attempting to treat each subtype
as discussed in this article. DN Conflict of interest Paula is also a Nurse Consultant/ Team Leader for Galderma (UK) Ltd. This article is not endorsed by Galderma (UK) Ltd. Dermatological Nursing, 2017, Vol 16, No 2 References 1. Wolf JE Rosacea: Diagnosis and management of a complex and significant disorder. Consultant 2016, 56(10) 901-905 2. Stollery N Managing patients with rosacea. MIMS Dermatology 2017, 13(1) 36-37 3. Plegwin G Kligman A Acne and Rosacea. 3rd Completely revised and enlarged edition. Springer New York 2000 p456 4. Holmes A D Steinhoff M Integrative concepts of rosacea pathophysiology, clinical presentation and new therapeutics. Experimental Dermatology 2016, 1-9 5. Steinhoff M, Vocanson M, Voegel J, Hacini-Rachinel F, Schafer G. Topical Ivermectin 10mg/g and oral Doxycycline 40mg Modified-release: Current evidence on the complementary use of anti-inflammatory Rosacea treatments. Adv Ther 2016, 33 1481-1501 6. Powell FC Rosacea Diagnosis and management. Informa
Healthcare 2009 Chapter 5 p69 7. Baldwin HE Diagnosis and treatment of Rosacea: state of the art. J Drugs and Dermatol 2012, 11(6) 725-30 8. Tan J, Almeida LMC, Bewley, A et al Updating the diagnosis, classification and assessment of roscea: recommendations from the global ROSacea COsensus (ROSCO) panel. British Journal of Dermatology 2017, 176 431-438 9. Primary Care Dermatology Society (PCDS) www.pcdsorguk [last accessed April 2017] 10. Changing Faces Charity www changingfaces.orguk [last accessed April 2017] 11. Walsh TR, Dreno B Antibiotic resistance in acne, an increasing topical and oral threat: a systemic review. The Lancet Infectious Diseases 2016, 16(3) 12. Moustafa et al The psychological impact of Rosacea and the influence of current management options. J Am Acad 2014, 71(5)973-80 13. Krasuska M, Millings A, Lavda A, Thompson A. Psychological needs and availability of support for people with Rosacea and Psoriasis findings from a GP survey. Dermatological Nursing 2016 15(2)
48-49 www.bdngorguk




 Írásunkban a műelemzések készítésének módszertanát járjuk körül. Foglalkozunk az elemzés főbb fajtáival, szempontjaival és tanácsokat adunk az elemzés legfontosabb tartalmi elemeivel kapcsolatban is. Módszertani útmutatónk főként tanulók számára készült!
Írásunkban a műelemzések készítésének módszertanát járjuk körül. Foglalkozunk az elemzés főbb fajtáival, szempontjaival és tanácsokat adunk az elemzés legfontosabb tartalmi elemeivel kapcsolatban is. Módszertani útmutatónk főként tanulók számára készült!