Datasheet
Year, pagecount:2004, 10 page(s)
Language:English
Downloads:12
Uploaded:November 25, 2011
Size:54 KB
Institution:
-
Comments:
Attachment:-
Download in PDF:Please log in!
Comments
No comments yet. You can be the first!
Most popular documents in this category
Content extract
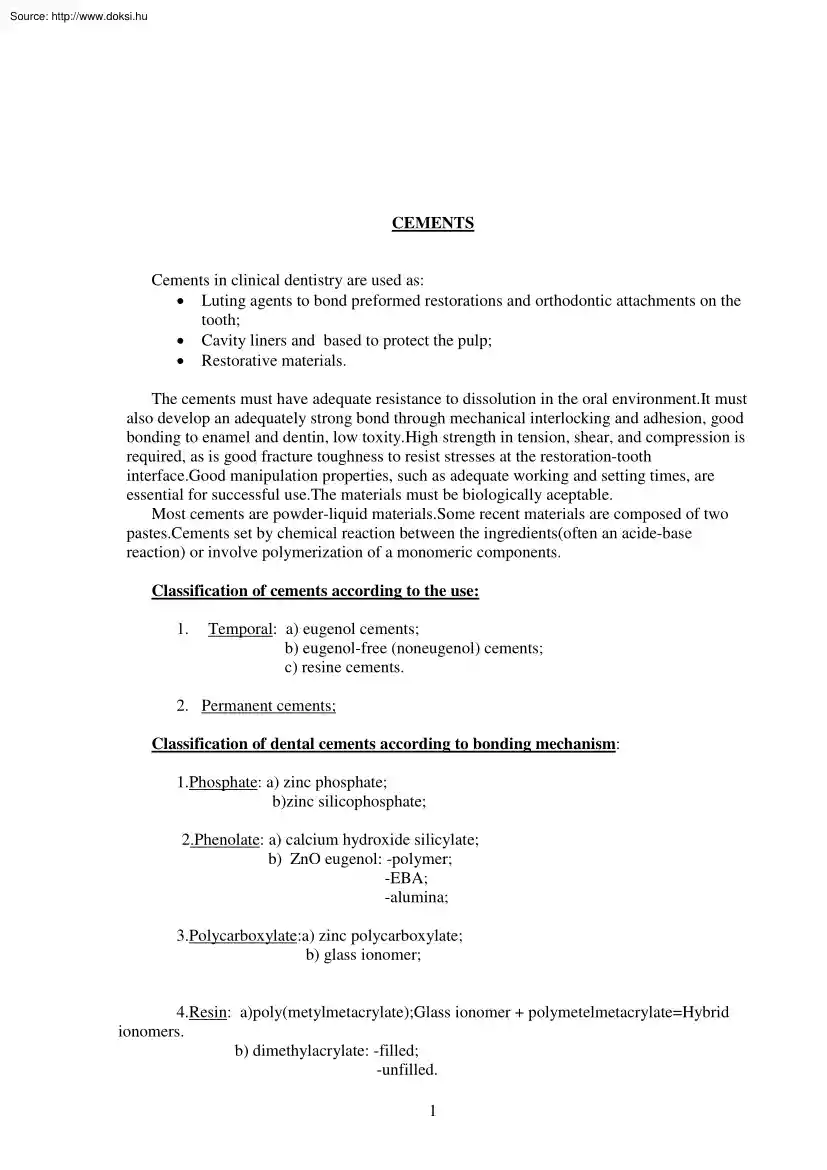
CEMENTS Cements in clinical dentistry are used as: • Luting agents to bond preformed restorations and orthodontic attachments on the tooth; • Cavity liners and based to protect the pulp; • Restorative materials. The cements must have adequate resistance to dissolution in the oral environment.It must also develop an adequately strong bond through mechanical interlocking and adhesion, good bonding to enamel and dentin, low toxity.High strength in tension, shear, and compression is required, as is good fracture toughness to resist stresses at the restoration-tooth interface.Good manipulation properties, such as adequate working and setting times, are essential for successful use.The materials must be biologically aceptable Most cements are powder-liquid materials.Some recent materials are composed of two pastes.Cements set by chemical reaction between the ingredients(often an acide-base reaction) or involve polymerization of a monomeric components. Classification of cements
according to the use: 1. Temporal: a) eugenol cements; b) eugenol-free (noneugenol) cements; c) resine cements. 2. Permanent cements; Classification of dental cements according to bonding mechanism: 1.Phosphate: a) zinc phosphate; b)zinc silicophosphate; 2.Phenolate: a) calcium hydroxide silicylate; b) ZnO eugenol: -polymer; -EBA; -alumina; 3.Polycarboxylate:a) zinc polycarboxylate; b) glass ionomer; 4.Resin: a)poly(metylmetacrylate);Glass ionomer + polymetelmetacrylate=Hybrid ionomers. b) dimethylacrylate: -filled; -unfilled. 1 Bonding mechanizm Nonadhesive luting The luting agent served primarily to fill the gap and prevent entrance of fluids.Zinc phisphate cement, for example, exibits no adhesion on the molecular levelIt holds the restoration in place by engaging small irregularities on the surfaces of both tooth and restoration.The nearly parellel opposing walls of a correctly prepared tooth without shearing or crushing the minute projections of cement extending into
reccesses in the surface. Micromechanical bonding.Resine cements have tensile strenhtgs in the range of 3040MPa, which is aproximately five times that of zinc phosphate cementsWhen used on pitted surfaces, they can provide effective micromechanical bonding.The tensile strength of such bonds can sometimes exceed the cohesive strength of enamel.This allows the use of less extensive tooth prepararion for restorations such as ceramic veneers and resin-bonded fixed partial dentures.The deep irregularities necessary for micromechanical bonding can be producted on enamel surface by etching with phosphoric acid solution or gel;on ceramic by etching with hydrofluoric acid, and on metals by electrolytic etching, chemical etching, sandblasting, or by incorporating salt crystals into the preliminary resin pattern. Molecular adhesion: Molecular adhesion involves physical forces( bipolar, Van der Walls andchemical bonds(ionic, covalent) between the molecules of two different substances.Newer
cements, such as polycarboxylate and glass ionomers, possess some adhesive capabilities, although this is limited by their relatively low cohesive strength.They still depend primarily on nearly parallel walls in the preparation to retain restorations.Limited success has been achieved in attempts to develop resin cements and coulping agents that will exhibit strong, durable molecular adhesion to tooth structure, base metals, and ceramic.Noble metal alloys are not well suited for direct molecular bonding.However, a thin layer of silane can be bonded to a gold alloy with spetial equipment to serve as a coupling agent by bonding chemically to resin cements.Equally effective is a layer of tin electroplated onto the gold alloy.By applying a silane coupler to roughened porcelain, shear bond strengths in excess of the cohesive etrength of the porcelain have been achieved in the laboratory.However,such bonds tend to become weaker after thermocycling in water.At this time, molecular adhesion
should be looked upon only as a way to anhance mechanical and micromechanical retention and reduce microleakage, rather than as an independent bonding mechanism. Phosphate-based cements 1.Phosphate: a) zinc phosphate; b)zinc silicophosphate; 2.Phenolate: a) calcium hydroxide silicylate; b) ZnO eugenol: -polymer; -EBA; -alumina; 3.Polycarboxylate:a) zinc polycarboxylate; b) glass ionomer; 2 4.Resin: a)poly(metylmetacrylate);Glass ionomer + polymetelmetacrylate=Hybrid ionomers. b) dimethylacrylate: -filled; -unfilled. The powder is ZnO with up to 10%MgO and small amount of pigments.The liquid is an aqueous solution of phosphoric acid containing 45-64% acid and 30-55% water also 2-3% Al Aluminum is essential to the cement-forming reaction.Some Zn-phosphate cements have modified composition(can contain calcium hydroxide,fluoride) At room temperature the working time is 3-6 minutes, the setting time is 5-14 minutes.Extended working time and shorter setting time can be achieved by use
of a cold mixing slab, which permits up to an aproximete 50% icrease in the amount of powder, improving both strength and resistance to dissolution.The tooth and restoration must be wet.The cement must flow into the regularities on the surface and seal the gap between tooth and restoration.Dissolution contributes to marginal leakage around restorations and bacteria penetration. The mixing slab must be dried before use.The powder ia aded to the liquid in small portions to achieve the desired consistency. Advantages: low cost high rigidity long working time easy to use Disadvantages: no bond to tooth Slow setting time Moisture sensitivity durin mixing Soluble in oral fluids Pulp irritation No fluoride release Modified zinc phosphate cements Copper and silver cements Black copper cements contain cupric oxide(CuO); red copper cements contain cuprous oxide(Cu2O).Others may contain cuprous iodide or silicateThese cements are much acidic resulting pulpar irritation.Their solubility is
higher and their strength is lower than zinc phosphate cements. Copper and silver cements Stannous fluoride (1% to 3%) is present in some orthodontic cementsThese matrials have a higher solubility and lower strength than zinc phosphate cements. Due to dissolution of the fluoride containing material.Fluoride uptake by enamel from such results in reduced enamel solubility and potentially anticariogenic effect. 3 Silicophosphate cement This cement is combination of zinc phosphate and silicate cements.it is used for cementation of fixed restorations and orthodontic bands, as a provisional posterior restorative material and as a dual-purpose material.The powder consists of 10%-20% zinc oxide and silicate glass.The silicate glass usually contains 12-25% fluorideSometimes can be small amount of mercury or silver.The liquid is a concentrated orthophosphoric acid solution cotaining about 45%water and 2-5%aluminum and zinc salts. The setting reaction: Zinc oxide/aluminosilicate+ phosphoric
acid= zinc aluminosilicate phosphate gel The set cement consists of unreacted glass and zinc oxide particles bonded together by the aluminosilico-phosphate gel matrix. The mixing is analogous to that for a phosphate cement;a nonabradable spatula and a cooled mixing slab should be used.The filling mix should be glossy, with puttylike consistency.The setting time is 5-7minutesWorking time is about 4 minutes and may be increased by using a cold mixing slab. The toughness and abrasion resistance are higher than those of phosphate cements.The solubility in organic acids and in the mouth is less thanfor phosphate cements.The fluoride is leached out and may contribute to anticariogenic action.The durability in bonding orthodontic bands to teeth is greater, and less decalcification is observed.The glass content gives greater translucency than phosphate cements,making silicophosphate cements useful for cementation of porcelain restorations.The pulpar protection is necessary on vital teeth
because the pH of this cement is 4-5. Advantages: better strength, toughness and abrasion resistancethan zinc phosphate cemenent; Fluoride release Translucency Low solubility Better bonding Disadvantages: low pH- increased pulp irritation Manipulation is more critical than with zinc phosphate cements. Phenolate-based cements Zinc oxide-eugenol cements Is used for provisional cementation of crowns and fixed partial dentures, and as a liner in deep cavity preparations. The powder is pure zinc oxide, can be small amount of fillers, such as silica.The liquid is purified eugenol or is some comertial materials, oil of cloves(85% eugenol).One percent of alcohol or acetic acid may be present to accelerate setting together with small amounts of water, which is essential to the setting reaction.A chemical reaction occurs between zinc oxide and eugenol, with the formation of zinc eugenolate(eugenate). 4 The zinc oxide is slowly wetted by the eugenol, therefore, prolonged and vigorous
spatulation is required, especially for a thick mix.A powder/ liquid racio of 3:1 or 4:1 must be used for maximum strength. The working time is long because moisture is required for seting.The set time is controlled by moisture availability, accelerators, and the powder/ liquid ratio.Mixes of cementing consistency sat very slowly unless accelerators are used and/ or a drop of water is added.The setting time is of 2 to 10 minutes ( depends on comercial brand)The compresive and tensile strength is very low.The solubility is highThe eugenol gives the anodyne and obtundent effect on pulp in the deep cavities.When exposed directly to oral conditions, the material maintains good sealing characteristics despite a volumetric shrinkage of 0.9% and thermal expansion.The sealing capacity and antibacterial action appear to facilitate pulpal healing;however, when in direct contact with connective tissues, the material is an irritant.Eugenol is potential allergen Advantages: anodyne and obtundent
effect to the pulp Good sealing ability Good resistance to marginal penetration Disadvantages: low strength and abrasion resistance Solubility and desintegration in oral fluids Little anticariogenic reaction Eugenol is allergen Reinforced zinc oxide-eugenol cements These materials have been used as cementing agents for crowns and fixed partial dentures, cavity liners and base materials and provisional restorative materials. The powder consists of zinc oxide with 10-40% finely divided natural or sunthetic resins( pine resin, poly methyl methecrylate, polystyrene, polycarbonate) together with acceslerators.The liquid is eugenol, which may also contain dissolved resins as mentioned earlier and accelerators such as acetic acid, as well as antimicrobial agents such thymol or 8hydroxyquinolineThe setting reaction is similar to zinc oxide eugenol cements.Acidic resins such as colophony(abietic acid) may react with the zinc oxide, stengthening the matrix.The powder is mixed into the liquid in
small portions with vigorous spatulation until the correct amount has been incorporated.Both powder and liquid containers should be kept closed and stored under dry conditions. These cements have long working time , because moisture is needed for setting.Setting time is also lengthened by reducing the powder/ liquid racio.The solubility of these cements is lower than of zinc oxide- eugenol cements.Sometimes these cements can have inflammatory reactions in connective tissue. Advantage: good sealing properties Disadvantages: low strength Higher solubility Higher desintegration compared with zinc oxide- eugenol cements Softening and discoloratio of some resin restorative materials EBA and other chelate cement EBA-ORTHO-ETHOXYBENZOIC CID. 5 These materials are used for cementation of inlays, crowns, and fixsed partial dentures, for provisional restorations, and as base or lining material. In EBA materials the powder is mainly zinc oxide containing 20-30%aluminum oxide or other mineral
fillers.Polymeric reinforcing agents, such as poly(methyl methacrylate), may also be present.The liquid consist of 50-66% ethoxybenzoic acid with the remainder eugenol.The setting mechanism : reaction between EBA, eugenol, and zinc oxide gives chelate salts. The cement mixes readily to a very fluid consistency even at a high powder/liquid ratio.The working time at room temperature is long because of the dependence on moisture.The setting time is ~7-13 minutes under oral conditionsThe solubility is similar to that of the polymer-reinforced zinc oxide- eugenol cements. Advantages: easy mixing Long working time Good flow characteristics Low irritation to the pulp Disadvantages: high solubility Poorer retention than zinc phosphate cements Calcium hydroxide chelate cements The value of calcium hydroxide as a pulp- capping material that facilitates the formation of reparative dentin has long been recognized.This action appears to be largely attributable to its alkaline pH and consequent
antibacterial and protein-lyzing effect.Although a number of aqueous paste materials based on calcium hydroxide are available, they are not easy to manipulate and the dried films tend to crack.The materials are used as iliners in deep cavity preparation.They are usually formulated as two pastes:one paste contains calcium hydrocide, zinc oxide, and zinc salts in ethylene toluene sulphonamide; the other contains calcium sulfate, titanium dioxide, and calcium tungstate(a radiopacifying agent) in a liquid disalicylate ester of butane-1,3-diol.The calcium hydroxide is intended to be in excess to produce an alkaline pH that will effect an antibacterial and remineralization action.These cements can contain fluoride. Calcium and zinc oxide react with the salicylate ester to form a chelate similar to the zinc oxide-eugenol reaction.The reaction is accelerated by moisture and accelerators Working time is 3-5 minutes.The setting time is about 1-2 minutesThe cement has good antibacterial and
remineralization properties. Advantages: easy to manipulate Rapid hardening in thin layers Good sealing characteristics Beneficial effects on carious dentine and exposed pulp. Disadvantages: low strength Low modulus of elasticity High marginal leakage Polycarboxylate( caroxylate) based cements 6 Zinc polycarboxylate cements Zinc polycarboxylates are used for the cementation of cast alloys and porcelain restorations and orthodontic bands, as cavity or base materials, and as provisional restorative materials. The powder in these cements is zinc oxide with, in some cases, 1-5% magnesium oxide;10%-40% aluminium oxide or other reinforcing fillers , fluoride may be too.The liquid is 40% aqueous solution of polyacrylic acid or an acrylic acid copolymer with other organic acids, such as itaconic acide.In some brands of the material the polyacrylic acid components is dried and added to the powder.The zinc oxide reacts with the polyacrylis acid, forming a cross-linked structure of zinc
polyacrylate. Zinc oxide +polycrylic acid=zinc polyacrylate The material should be carefully proportioned and the freshly dispensed components mixed rapidly in 30- 40 seconds.The powder and liquid should be stored under cool conditions.The working time is 25-35 minutes, the setting time is 6-9 minutesThe working time can be increased by mixing the material on a cold slab and by refrigerating the powder. The solubility is less than that for zinc phosphate cements.Bonding to clean enamel and dentin surfaces can occur through calcium complexation.In practise, adhesion to dentine may be limited because of debris and contamination.The material also sticks to clean stainless steel, amalgam, chromium- cobalt, and other alloys. Advantages: low irritation Adhesion to tooth structure and alloys Easy manipulation High strength Low solubility Fluoride release Disadvantages: must be accurate proportioning for optimal properties Low compressive strength Short working time Glass-ionomer cements
These cements are used for the cementation of cast-alloys and porcelain restorations and orthodontic bands, as cavity or base materials, and as restorative materials, especially for erosion lesion.They are being replaced by hybrid ionomer cements, which allow better handling. The powder contains calcium aluminum fluorosilicate glass a particles size around 40 am for the filling materials and less than 25 am for the looting materials. For improving physical properties can be added silver powder, zinc oxide. The liquid is 50% aqueous solution of polyacrylic-itaconic acide or other polycarboxylic acid copolymer.In some materials the solid copolymer is added to the powder, and the solution contains tartaric acid; in other, all ingredients are in the powder, and the liquid is water. The polyacrylic and tartaric acids react with the glass, leaching calcium and aluminum ions from the surface, which cross-link the polyacid molecules into a gel. The mixing should be on cold slab, powder and
liquid should be chilled. The restorative cement should have puttylike consistency and a glossy surface Tooth surface must be clean, free from saliva but not dehydrated. The restoration margins or filling surfaces should be protected with a varnish or a light- curing sealant. 7 The setting time is 3-4minutes.Materials that are light- cured set in 30 secondsGood resistance to dissolution and solubility is improved by varnish protection.Glass- ionomers exibit bonding to enamel, dentin, and alloys.The low pH of these cements is prolonged, so it can lead to pulpal sensitivity. Advantages: easy mixing Good seal Fluoride release Adequate strength Good adhesive properties Translucency Disadvantages: pulpal sensitivity Slow setting time Moisture sensitivity. Resin modified glass-ionomer cements Sometimes they are called hybrid ionomers. Have many uses: liners, bases, core buildups, and luting cements. One hybrid ionomer is used for permanent cementation of crowns, orthodontic appliances,
and core buildups. In hybrid ionomers, the acid- base setting reaction in glass-ionomer cements has been modified by the introduction of water-soluble polymers and polymerizable monomers into the composition.The use of copolymers of acrylic acid and methacrylate monomers in the liquid leads to materials that undergo the customary acid-base reaction on setting and can also be light cured via the methacrylate groups.Resine modified glass- ionomer cements are available in hand- mixed and predosed capsules.The resine monomers in the liquid depend on the product and include bis-GMA, hydroxyethylmethacrylate, and others. The powder and liquid should be mixed quickly(30seconds).Working time is ~25 minutes.Absorbtion of water is more than for resine cementsHybride ionomers are not recommended for luting all- ceramic crowns, to avoid possible expantion stresses and crown fracture.Hybride ionomers release fluoride from the glass components Advantages: dual cure Fluoride release Higher flexural
strength than glass-ionomer cements Easy to handling Good bonding Disadvantage: setting expantion Polymer-based cements There are two types: 1)materials based on methyl methacrylate, 2) materials based on aromatic dimethacrylates of the bis-GMA type. Acrylic resin cements Acrylic resin cements are used for the cementation of restorations, provisional crowns. 8 The powder in these materials is a finely divided methyl methacrylate polymer or copolymer containing benzoyl peroxide as the initiator,mineral filler and pigments may be also present.The liquid is a methyl methacrylate monomer containing an amine accelerator.The set mass consists of the new polymer matrix uniting the undissolved but swollen original polymer granules. The liquid is added to powder with minimal spatulation to avoid an incorporation of air. Working time is short. These cements are stronger and less soluble than other types of cements, but have low rigidity. They have no effective bond to tooth structure in the
presence of moisture; thus they permit marginal leakage, although they may show better bonding than other cements to resin facings and polycarbonate crowns. Advantages: low solubility High strength Disadvantages: short working time Pulpal sensitivity Difficult to remove the excess of cement from mergins Adhesive resin cements These cements are used for cementation of metal fixed partial dentures (especially of base metals) and for bonding amalgam to dentin and composites. Chemical composition: 4META +methyl methacrylate monomer(as an additional polymerization initiator), tributyl boron( important for chemical bonding to dentine). The physical properties are typical of acrylic resins. Dimethacrylate cements These cements are based on bis-GMS system. They are combination of an aromatic dimethacrylate with other monomers containing various amounts of ceramic filler. The cements are used for bonding crowns(usually porcelain), fixed partial dentures, inlays, veneers and indirect resin
restorations. The cements are classified according to the methods of curing: 1.Chemically(or auto) cured These are usually paste- paste systems and are used ti cement metal and opaque ceramic core(Procera, In-Ceram) restorations. 2.Dual cured:These cements start curing with light and continue with chemical curung. The chemical cure will polymerize more thoroughly than light curing alone There are used to cement translucent restorations(porcelain, indirect resin restorations) 3.Light cured/ dual cured: These can be used for light curing only or can be dual cured when dual-cure catalysts are added to the light- cure base. These products are used for both light- cure applications(thin porcelain veneer) and dual-cure applications. In the powder- liquid material, the powder is generally a finely divided borosilicate or silica glass together with fine polymer powder and an organic peroxide initiator.he liquid is a mixture of bis- GMA and/ or other dimethacrylate monomers containing an amine
promoter for polymerization.Paste materials are proportioned 1:1 9 Advantages: high strength Low oral solubility High micromechanical(and possible chemical)bonding to enamel, dentin, ceramic Good esthetics Disadvantages: short working time Negative effect on pulp Difficult to remove the excess of cement from margins. . 10
according to the use: 1. Temporal: a) eugenol cements; b) eugenol-free (noneugenol) cements; c) resine cements. 2. Permanent cements; Classification of dental cements according to bonding mechanism: 1.Phosphate: a) zinc phosphate; b)zinc silicophosphate; 2.Phenolate: a) calcium hydroxide silicylate; b) ZnO eugenol: -polymer; -EBA; -alumina; 3.Polycarboxylate:a) zinc polycarboxylate; b) glass ionomer; 4.Resin: a)poly(metylmetacrylate);Glass ionomer + polymetelmetacrylate=Hybrid ionomers. b) dimethylacrylate: -filled; -unfilled. 1 Bonding mechanizm Nonadhesive luting The luting agent served primarily to fill the gap and prevent entrance of fluids.Zinc phisphate cement, for example, exibits no adhesion on the molecular levelIt holds the restoration in place by engaging small irregularities on the surfaces of both tooth and restoration.The nearly parellel opposing walls of a correctly prepared tooth without shearing or crushing the minute projections of cement extending into
reccesses in the surface. Micromechanical bonding.Resine cements have tensile strenhtgs in the range of 3040MPa, which is aproximately five times that of zinc phosphate cementsWhen used on pitted surfaces, they can provide effective micromechanical bonding.The tensile strength of such bonds can sometimes exceed the cohesive strength of enamel.This allows the use of less extensive tooth prepararion for restorations such as ceramic veneers and resin-bonded fixed partial dentures.The deep irregularities necessary for micromechanical bonding can be producted on enamel surface by etching with phosphoric acid solution or gel;on ceramic by etching with hydrofluoric acid, and on metals by electrolytic etching, chemical etching, sandblasting, or by incorporating salt crystals into the preliminary resin pattern. Molecular adhesion: Molecular adhesion involves physical forces( bipolar, Van der Walls andchemical bonds(ionic, covalent) between the molecules of two different substances.Newer
cements, such as polycarboxylate and glass ionomers, possess some adhesive capabilities, although this is limited by their relatively low cohesive strength.They still depend primarily on nearly parallel walls in the preparation to retain restorations.Limited success has been achieved in attempts to develop resin cements and coulping agents that will exhibit strong, durable molecular adhesion to tooth structure, base metals, and ceramic.Noble metal alloys are not well suited for direct molecular bonding.However, a thin layer of silane can be bonded to a gold alloy with spetial equipment to serve as a coupling agent by bonding chemically to resin cements.Equally effective is a layer of tin electroplated onto the gold alloy.By applying a silane coupler to roughened porcelain, shear bond strengths in excess of the cohesive etrength of the porcelain have been achieved in the laboratory.However,such bonds tend to become weaker after thermocycling in water.At this time, molecular adhesion
should be looked upon only as a way to anhance mechanical and micromechanical retention and reduce microleakage, rather than as an independent bonding mechanism. Phosphate-based cements 1.Phosphate: a) zinc phosphate; b)zinc silicophosphate; 2.Phenolate: a) calcium hydroxide silicylate; b) ZnO eugenol: -polymer; -EBA; -alumina; 3.Polycarboxylate:a) zinc polycarboxylate; b) glass ionomer; 2 4.Resin: a)poly(metylmetacrylate);Glass ionomer + polymetelmetacrylate=Hybrid ionomers. b) dimethylacrylate: -filled; -unfilled. The powder is ZnO with up to 10%MgO and small amount of pigments.The liquid is an aqueous solution of phosphoric acid containing 45-64% acid and 30-55% water also 2-3% Al Aluminum is essential to the cement-forming reaction.Some Zn-phosphate cements have modified composition(can contain calcium hydroxide,fluoride) At room temperature the working time is 3-6 minutes, the setting time is 5-14 minutes.Extended working time and shorter setting time can be achieved by use
of a cold mixing slab, which permits up to an aproximete 50% icrease in the amount of powder, improving both strength and resistance to dissolution.The tooth and restoration must be wet.The cement must flow into the regularities on the surface and seal the gap between tooth and restoration.Dissolution contributes to marginal leakage around restorations and bacteria penetration. The mixing slab must be dried before use.The powder ia aded to the liquid in small portions to achieve the desired consistency. Advantages: low cost high rigidity long working time easy to use Disadvantages: no bond to tooth Slow setting time Moisture sensitivity durin mixing Soluble in oral fluids Pulp irritation No fluoride release Modified zinc phosphate cements Copper and silver cements Black copper cements contain cupric oxide(CuO); red copper cements contain cuprous oxide(Cu2O).Others may contain cuprous iodide or silicateThese cements are much acidic resulting pulpar irritation.Their solubility is
higher and their strength is lower than zinc phosphate cements. Copper and silver cements Stannous fluoride (1% to 3%) is present in some orthodontic cementsThese matrials have a higher solubility and lower strength than zinc phosphate cements. Due to dissolution of the fluoride containing material.Fluoride uptake by enamel from such results in reduced enamel solubility and potentially anticariogenic effect. 3 Silicophosphate cement This cement is combination of zinc phosphate and silicate cements.it is used for cementation of fixed restorations and orthodontic bands, as a provisional posterior restorative material and as a dual-purpose material.The powder consists of 10%-20% zinc oxide and silicate glass.The silicate glass usually contains 12-25% fluorideSometimes can be small amount of mercury or silver.The liquid is a concentrated orthophosphoric acid solution cotaining about 45%water and 2-5%aluminum and zinc salts. The setting reaction: Zinc oxide/aluminosilicate+ phosphoric
acid= zinc aluminosilicate phosphate gel The set cement consists of unreacted glass and zinc oxide particles bonded together by the aluminosilico-phosphate gel matrix. The mixing is analogous to that for a phosphate cement;a nonabradable spatula and a cooled mixing slab should be used.The filling mix should be glossy, with puttylike consistency.The setting time is 5-7minutesWorking time is about 4 minutes and may be increased by using a cold mixing slab. The toughness and abrasion resistance are higher than those of phosphate cements.The solubility in organic acids and in the mouth is less thanfor phosphate cements.The fluoride is leached out and may contribute to anticariogenic action.The durability in bonding orthodontic bands to teeth is greater, and less decalcification is observed.The glass content gives greater translucency than phosphate cements,making silicophosphate cements useful for cementation of porcelain restorations.The pulpar protection is necessary on vital teeth
because the pH of this cement is 4-5. Advantages: better strength, toughness and abrasion resistancethan zinc phosphate cemenent; Fluoride release Translucency Low solubility Better bonding Disadvantages: low pH- increased pulp irritation Manipulation is more critical than with zinc phosphate cements. Phenolate-based cements Zinc oxide-eugenol cements Is used for provisional cementation of crowns and fixed partial dentures, and as a liner in deep cavity preparations. The powder is pure zinc oxide, can be small amount of fillers, such as silica.The liquid is purified eugenol or is some comertial materials, oil of cloves(85% eugenol).One percent of alcohol or acetic acid may be present to accelerate setting together with small amounts of water, which is essential to the setting reaction.A chemical reaction occurs between zinc oxide and eugenol, with the formation of zinc eugenolate(eugenate). 4 The zinc oxide is slowly wetted by the eugenol, therefore, prolonged and vigorous
spatulation is required, especially for a thick mix.A powder/ liquid racio of 3:1 or 4:1 must be used for maximum strength. The working time is long because moisture is required for seting.The set time is controlled by moisture availability, accelerators, and the powder/ liquid ratio.Mixes of cementing consistency sat very slowly unless accelerators are used and/ or a drop of water is added.The setting time is of 2 to 10 minutes ( depends on comercial brand)The compresive and tensile strength is very low.The solubility is highThe eugenol gives the anodyne and obtundent effect on pulp in the deep cavities.When exposed directly to oral conditions, the material maintains good sealing characteristics despite a volumetric shrinkage of 0.9% and thermal expansion.The sealing capacity and antibacterial action appear to facilitate pulpal healing;however, when in direct contact with connective tissues, the material is an irritant.Eugenol is potential allergen Advantages: anodyne and obtundent
effect to the pulp Good sealing ability Good resistance to marginal penetration Disadvantages: low strength and abrasion resistance Solubility and desintegration in oral fluids Little anticariogenic reaction Eugenol is allergen Reinforced zinc oxide-eugenol cements These materials have been used as cementing agents for crowns and fixed partial dentures, cavity liners and base materials and provisional restorative materials. The powder consists of zinc oxide with 10-40% finely divided natural or sunthetic resins( pine resin, poly methyl methecrylate, polystyrene, polycarbonate) together with acceslerators.The liquid is eugenol, which may also contain dissolved resins as mentioned earlier and accelerators such as acetic acid, as well as antimicrobial agents such thymol or 8hydroxyquinolineThe setting reaction is similar to zinc oxide eugenol cements.Acidic resins such as colophony(abietic acid) may react with the zinc oxide, stengthening the matrix.The powder is mixed into the liquid in
small portions with vigorous spatulation until the correct amount has been incorporated.Both powder and liquid containers should be kept closed and stored under dry conditions. These cements have long working time , because moisture is needed for setting.Setting time is also lengthened by reducing the powder/ liquid racio.The solubility of these cements is lower than of zinc oxide- eugenol cements.Sometimes these cements can have inflammatory reactions in connective tissue. Advantage: good sealing properties Disadvantages: low strength Higher solubility Higher desintegration compared with zinc oxide- eugenol cements Softening and discoloratio of some resin restorative materials EBA and other chelate cement EBA-ORTHO-ETHOXYBENZOIC CID. 5 These materials are used for cementation of inlays, crowns, and fixsed partial dentures, for provisional restorations, and as base or lining material. In EBA materials the powder is mainly zinc oxide containing 20-30%aluminum oxide or other mineral
fillers.Polymeric reinforcing agents, such as poly(methyl methacrylate), may also be present.The liquid consist of 50-66% ethoxybenzoic acid with the remainder eugenol.The setting mechanism : reaction between EBA, eugenol, and zinc oxide gives chelate salts. The cement mixes readily to a very fluid consistency even at a high powder/liquid ratio.The working time at room temperature is long because of the dependence on moisture.The setting time is ~7-13 minutes under oral conditionsThe solubility is similar to that of the polymer-reinforced zinc oxide- eugenol cements. Advantages: easy mixing Long working time Good flow characteristics Low irritation to the pulp Disadvantages: high solubility Poorer retention than zinc phosphate cements Calcium hydroxide chelate cements The value of calcium hydroxide as a pulp- capping material that facilitates the formation of reparative dentin has long been recognized.This action appears to be largely attributable to its alkaline pH and consequent
antibacterial and protein-lyzing effect.Although a number of aqueous paste materials based on calcium hydroxide are available, they are not easy to manipulate and the dried films tend to crack.The materials are used as iliners in deep cavity preparation.They are usually formulated as two pastes:one paste contains calcium hydrocide, zinc oxide, and zinc salts in ethylene toluene sulphonamide; the other contains calcium sulfate, titanium dioxide, and calcium tungstate(a radiopacifying agent) in a liquid disalicylate ester of butane-1,3-diol.The calcium hydroxide is intended to be in excess to produce an alkaline pH that will effect an antibacterial and remineralization action.These cements can contain fluoride. Calcium and zinc oxide react with the salicylate ester to form a chelate similar to the zinc oxide-eugenol reaction.The reaction is accelerated by moisture and accelerators Working time is 3-5 minutes.The setting time is about 1-2 minutesThe cement has good antibacterial and
remineralization properties. Advantages: easy to manipulate Rapid hardening in thin layers Good sealing characteristics Beneficial effects on carious dentine and exposed pulp. Disadvantages: low strength Low modulus of elasticity High marginal leakage Polycarboxylate( caroxylate) based cements 6 Zinc polycarboxylate cements Zinc polycarboxylates are used for the cementation of cast alloys and porcelain restorations and orthodontic bands, as cavity or base materials, and as provisional restorative materials. The powder in these cements is zinc oxide with, in some cases, 1-5% magnesium oxide;10%-40% aluminium oxide or other reinforcing fillers , fluoride may be too.The liquid is 40% aqueous solution of polyacrylic acid or an acrylic acid copolymer with other organic acids, such as itaconic acide.In some brands of the material the polyacrylic acid components is dried and added to the powder.The zinc oxide reacts with the polyacrylis acid, forming a cross-linked structure of zinc
polyacrylate. Zinc oxide +polycrylic acid=zinc polyacrylate The material should be carefully proportioned and the freshly dispensed components mixed rapidly in 30- 40 seconds.The powder and liquid should be stored under cool conditions.The working time is 25-35 minutes, the setting time is 6-9 minutesThe working time can be increased by mixing the material on a cold slab and by refrigerating the powder. The solubility is less than that for zinc phosphate cements.Bonding to clean enamel and dentin surfaces can occur through calcium complexation.In practise, adhesion to dentine may be limited because of debris and contamination.The material also sticks to clean stainless steel, amalgam, chromium- cobalt, and other alloys. Advantages: low irritation Adhesion to tooth structure and alloys Easy manipulation High strength Low solubility Fluoride release Disadvantages: must be accurate proportioning for optimal properties Low compressive strength Short working time Glass-ionomer cements
These cements are used for the cementation of cast-alloys and porcelain restorations and orthodontic bands, as cavity or base materials, and as restorative materials, especially for erosion lesion.They are being replaced by hybrid ionomer cements, which allow better handling. The powder contains calcium aluminum fluorosilicate glass a particles size around 40 am for the filling materials and less than 25 am for the looting materials. For improving physical properties can be added silver powder, zinc oxide. The liquid is 50% aqueous solution of polyacrylic-itaconic acide or other polycarboxylic acid copolymer.In some materials the solid copolymer is added to the powder, and the solution contains tartaric acid; in other, all ingredients are in the powder, and the liquid is water. The polyacrylic and tartaric acids react with the glass, leaching calcium and aluminum ions from the surface, which cross-link the polyacid molecules into a gel. The mixing should be on cold slab, powder and
liquid should be chilled. The restorative cement should have puttylike consistency and a glossy surface Tooth surface must be clean, free from saliva but not dehydrated. The restoration margins or filling surfaces should be protected with a varnish or a light- curing sealant. 7 The setting time is 3-4minutes.Materials that are light- cured set in 30 secondsGood resistance to dissolution and solubility is improved by varnish protection.Glass- ionomers exibit bonding to enamel, dentin, and alloys.The low pH of these cements is prolonged, so it can lead to pulpal sensitivity. Advantages: easy mixing Good seal Fluoride release Adequate strength Good adhesive properties Translucency Disadvantages: pulpal sensitivity Slow setting time Moisture sensitivity. Resin modified glass-ionomer cements Sometimes they are called hybrid ionomers. Have many uses: liners, bases, core buildups, and luting cements. One hybrid ionomer is used for permanent cementation of crowns, orthodontic appliances,
and core buildups. In hybrid ionomers, the acid- base setting reaction in glass-ionomer cements has been modified by the introduction of water-soluble polymers and polymerizable monomers into the composition.The use of copolymers of acrylic acid and methacrylate monomers in the liquid leads to materials that undergo the customary acid-base reaction on setting and can also be light cured via the methacrylate groups.Resine modified glass- ionomer cements are available in hand- mixed and predosed capsules.The resine monomers in the liquid depend on the product and include bis-GMA, hydroxyethylmethacrylate, and others. The powder and liquid should be mixed quickly(30seconds).Working time is ~25 minutes.Absorbtion of water is more than for resine cementsHybride ionomers are not recommended for luting all- ceramic crowns, to avoid possible expantion stresses and crown fracture.Hybride ionomers release fluoride from the glass components Advantages: dual cure Fluoride release Higher flexural
strength than glass-ionomer cements Easy to handling Good bonding Disadvantage: setting expantion Polymer-based cements There are two types: 1)materials based on methyl methacrylate, 2) materials based on aromatic dimethacrylates of the bis-GMA type. Acrylic resin cements Acrylic resin cements are used for the cementation of restorations, provisional crowns. 8 The powder in these materials is a finely divided methyl methacrylate polymer or copolymer containing benzoyl peroxide as the initiator,mineral filler and pigments may be also present.The liquid is a methyl methacrylate monomer containing an amine accelerator.The set mass consists of the new polymer matrix uniting the undissolved but swollen original polymer granules. The liquid is added to powder with minimal spatulation to avoid an incorporation of air. Working time is short. These cements are stronger and less soluble than other types of cements, but have low rigidity. They have no effective bond to tooth structure in the
presence of moisture; thus they permit marginal leakage, although they may show better bonding than other cements to resin facings and polycarbonate crowns. Advantages: low solubility High strength Disadvantages: short working time Pulpal sensitivity Difficult to remove the excess of cement from mergins Adhesive resin cements These cements are used for cementation of metal fixed partial dentures (especially of base metals) and for bonding amalgam to dentin and composites. Chemical composition: 4META +methyl methacrylate monomer(as an additional polymerization initiator), tributyl boron( important for chemical bonding to dentine). The physical properties are typical of acrylic resins. Dimethacrylate cements These cements are based on bis-GMS system. They are combination of an aromatic dimethacrylate with other monomers containing various amounts of ceramic filler. The cements are used for bonding crowns(usually porcelain), fixed partial dentures, inlays, veneers and indirect resin
restorations. The cements are classified according to the methods of curing: 1.Chemically(or auto) cured These are usually paste- paste systems and are used ti cement metal and opaque ceramic core(Procera, In-Ceram) restorations. 2.Dual cured:These cements start curing with light and continue with chemical curung. The chemical cure will polymerize more thoroughly than light curing alone There are used to cement translucent restorations(porcelain, indirect resin restorations) 3.Light cured/ dual cured: These can be used for light curing only or can be dual cured when dual-cure catalysts are added to the light- cure base. These products are used for both light- cure applications(thin porcelain veneer) and dual-cure applications. In the powder- liquid material, the powder is generally a finely divided borosilicate or silica glass together with fine polymer powder and an organic peroxide initiator.he liquid is a mixture of bis- GMA and/ or other dimethacrylate monomers containing an amine
promoter for polymerization.Paste materials are proportioned 1:1 9 Advantages: high strength Low oral solubility High micromechanical(and possible chemical)bonding to enamel, dentin, ceramic Good esthetics Disadvantages: short working time Negative effect on pulp Difficult to remove the excess of cement from margins. . 10



 Just like you draw up a plan when you’re going to war, building a house, or even going on vacation, you need to draw up a plan for your business. This tutorial will help you to clearly see where you are and make it possible to understand where you’re going.
Just like you draw up a plan when you’re going to war, building a house, or even going on vacation, you need to draw up a plan for your business. This tutorial will help you to clearly see where you are and make it possible to understand where you’re going.