A doksi online olvasásához kérlek jelentkezz be!
A doksi online olvasásához kérlek jelentkezz be!
Nincs még értékelés. Legyél Te az első!
Tartalmi kivonat
Source: http://www.doksinet Breast Reconstruction in the Obese Patient Elisabeth K. Beahm MD, FACS, Robert L Walton MD, FACS and David W Chang MD,FACS INTRODUCTION: Obesity has become a nationwide epidemic. The obese patient presents a highly problematic, yet growing population of patients presenting for breast reconstruction. Donor and recipient complications with autologous flaps appear to be higher in this group, leading some authors to recommended implant reconstruction in these patients, yet prosthetic options are limited due to inadequate size and shape.1-9 (Figures 1 and 2) A number of surgeons refuse to operate or limit their options for breast reconstruction in the very obese patient due to the potential for high complication rates. While unfavorable outcomes have stifled interest in breast reconstruction in the very obese, objective criteria are generally lacking. Currently there are no established clinical recommendations to objectively guide decision making for breast
reconstruction in the very obese patient. METHODS: A retrospective review of outcomes of breast reconstruction in obese patients was conducted over a 15 year period (1/1/1990 to 1/1/2005). Analysis criteria utilized stratified Body Mass Indices (BMI) (25-29.9, 30-349, 35-399, and >40) These patients were matched to normal weight patients (BMI < 24.9) by age and type of reconstruction including autologous flaps from the lower abdominal wall (Transverse Rectus Myocutaneous (TRAM), Deep inferior Epigastric (DIEP) and Superficial Inferior Epigastric (SIEA) flaps); Latissimus Dorsi (LD) flaps (with and without implants), and implant only methods. Outcomes analysis included assessment of complications including: fat necrosis, flap loss (total or partial), delayed wound healing (donor and/or recipient sites) abdominal wall complications in TRAM flap patients such as chronic pain, bulge, hernia, infection; length of hospital stay and medical complications such as Pulmonary embolus(PE)
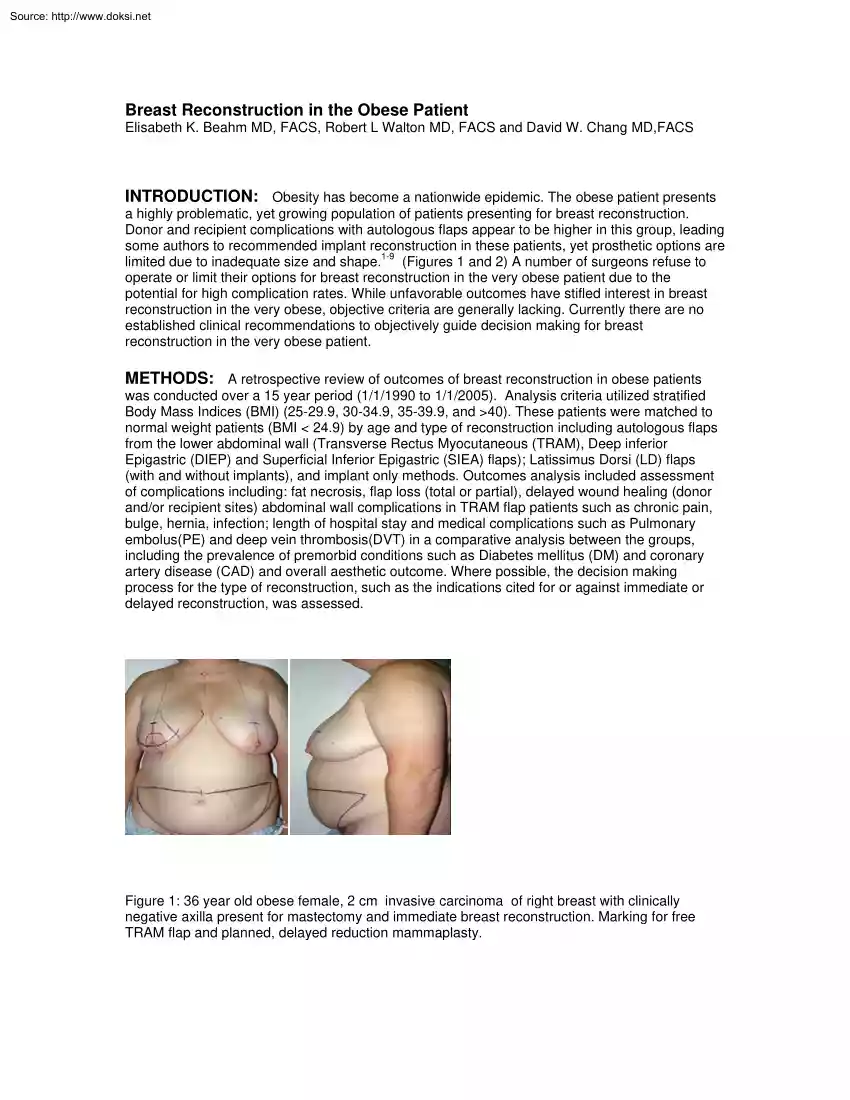
and deep vein thrombosis(DVT) in a comparative analysis between the groups, including the prevalence of premorbid conditions such as Diabetes mellitus (DM) and coronary artery disease (CAD) and overall aesthetic outcome. Where possible, the decision making process for the type of reconstruction, such as the indications cited for or against immediate or delayed reconstruction, was assessed. Figure 1: 36 year old obese female, 2 cm invasive carcinoma of right breast with clinically negative axilla present for mastectomy and immediate breast reconstruction. Marking for free TRAM flap and planned, delayed reduction mammaplasty. Source: http://www.doksinet RESULTS: The BMI in 3518 study patients ranged from 15.2 to 599 The mean BMI of the patients treated was noted to increase annually (24.2 to 268) over the study period The complication rate was comparable for all the BMI indices <35. In patients with a BMI ≥35 a significant increase in post-operative complications was noted in
all methods of reconstruction. Complication rates: 50% vs. 34% (TRAM); 333% vs 225% (Implant); 40% vs 33 %( LD); Overall 39% vs. 309% While complications increased with patients with a BMI over 35 and approached 100% in those with a BMI over 40 there was no linear correlation in this relationship. In a focused study of patients from 2000-2005 assessment of patient satisfaction and overall aesthetic outcome was deemed lower in patients presenting for breast reconstruction with a BMI ≥ 35. CONCLUSION: We have demonstrated an increased post-operative complication rate following breast reconstruction in patients with a BMI ≥35 compared to patients having a BMI <35. Reconstructive outcome satisfaction rates in these massively obese patients also appear to be low compared to breast reconstruction in thinner patients. These data provide argument for reassessing our approach to management of breast defects in obese patients having a BMI >35. Prospective study is warranted to
develop an appropriate treatment algorithm that will optimize surgical outcomes in this select patient group. Figure 2: Same patient seen in figure 1. Final pathology revealed 5 positive axillary lymph nodes Patient underwent post operative radiation therapy. Final post operative result seen 3 years after tailoring of the reconstruction, nipple areolar reconstruction and contralateral reduction mammaplasty. Source: http://www.doksinet REFERENCES: 1. Ducic I, Spear SL, Cuovo F, Hannan C Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: a 10-year analysis. Ann Plast Surg, 55(6);559-64; 2005. 2. Wang HT, Hartzell T, Olbrich KC, Erdmann D, Georgiade GS Delay of transverse rectus abdominis myocutaneous flap reconstruction improves flap reliability in the obese patient. Plast Reconstr Surg, 116(2);613-8; Discussion, 619-20; 2005. 3. Gabbay JS, Eby JB, Kulber DA The midabdominal TRAM flap for breast reconstruction in
morbidly obese patients. Plast Reconstr Surg, 115(3);764-70; 2005 4. Garvey PB, Buchel EW, Pockaj BA, Gray RJ, Samson TD The deep inferior epigastric perforator flap for breast reconstruction in overweight and obese patients. Plast Reconstr Surg, 115(2);447-57; 2005. 5. Moran SL, Serletti JM Outcome comparison between free and pedicled TRAM flap breast reconstruction in the obese patient. Plast Reconstr Surg, 108(7);1954-60; 2001 6. Lin KY, Johns FR, Gibson J, Long M, Drake DB, Moore MM An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol, 8(7);586-91; 2001. 7. Chang DW, Wang B, Robb GL, Reece GP, Miller MJ, Evans GR, Langstein HN, Kroll SS Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg, 105(5);1640-8; 2000 8. Disa JJ, Ad-El DD, Cohen SM, Cordeiro PG, Hidalgo DA The premature removal of tissue expanders in breast
reconstruction. Plast Reconstr Surg, 104(6);1662-5; 1999 9. Paige KT, Bostwick J 3rd, Bried JT, Jones G A comparison of morbidity from bilateral, unipedicled and unilateral, unipdicled TRAM flap breast reconstructions. Plast Reconstr Surg, 101(7);1819-27, 1998
reconstruction in the very obese patient. METHODS: A retrospective review of outcomes of breast reconstruction in obese patients was conducted over a 15 year period (1/1/1990 to 1/1/2005). Analysis criteria utilized stratified Body Mass Indices (BMI) (25-29.9, 30-349, 35-399, and >40) These patients were matched to normal weight patients (BMI < 24.9) by age and type of reconstruction including autologous flaps from the lower abdominal wall (Transverse Rectus Myocutaneous (TRAM), Deep inferior Epigastric (DIEP) and Superficial Inferior Epigastric (SIEA) flaps); Latissimus Dorsi (LD) flaps (with and without implants), and implant only methods. Outcomes analysis included assessment of complications including: fat necrosis, flap loss (total or partial), delayed wound healing (donor and/or recipient sites) abdominal wall complications in TRAM flap patients such as chronic pain, bulge, hernia, infection; length of hospital stay and medical complications such as Pulmonary embolus(PE)
and deep vein thrombosis(DVT) in a comparative analysis between the groups, including the prevalence of premorbid conditions such as Diabetes mellitus (DM) and coronary artery disease (CAD) and overall aesthetic outcome. Where possible, the decision making process for the type of reconstruction, such as the indications cited for or against immediate or delayed reconstruction, was assessed. Figure 1: 36 year old obese female, 2 cm invasive carcinoma of right breast with clinically negative axilla present for mastectomy and immediate breast reconstruction. Marking for free TRAM flap and planned, delayed reduction mammaplasty. Source: http://www.doksinet RESULTS: The BMI in 3518 study patients ranged from 15.2 to 599 The mean BMI of the patients treated was noted to increase annually (24.2 to 268) over the study period The complication rate was comparable for all the BMI indices <35. In patients with a BMI ≥35 a significant increase in post-operative complications was noted in
all methods of reconstruction. Complication rates: 50% vs. 34% (TRAM); 333% vs 225% (Implant); 40% vs 33 %( LD); Overall 39% vs. 309% While complications increased with patients with a BMI over 35 and approached 100% in those with a BMI over 40 there was no linear correlation in this relationship. In a focused study of patients from 2000-2005 assessment of patient satisfaction and overall aesthetic outcome was deemed lower in patients presenting for breast reconstruction with a BMI ≥ 35. CONCLUSION: We have demonstrated an increased post-operative complication rate following breast reconstruction in patients with a BMI ≥35 compared to patients having a BMI <35. Reconstructive outcome satisfaction rates in these massively obese patients also appear to be low compared to breast reconstruction in thinner patients. These data provide argument for reassessing our approach to management of breast defects in obese patients having a BMI >35. Prospective study is warranted to
develop an appropriate treatment algorithm that will optimize surgical outcomes in this select patient group. Figure 2: Same patient seen in figure 1. Final pathology revealed 5 positive axillary lymph nodes Patient underwent post operative radiation therapy. Final post operative result seen 3 years after tailoring of the reconstruction, nipple areolar reconstruction and contralateral reduction mammaplasty. Source: http://www.doksinet REFERENCES: 1. Ducic I, Spear SL, Cuovo F, Hannan C Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: a 10-year analysis. Ann Plast Surg, 55(6);559-64; 2005. 2. Wang HT, Hartzell T, Olbrich KC, Erdmann D, Georgiade GS Delay of transverse rectus abdominis myocutaneous flap reconstruction improves flap reliability in the obese patient. Plast Reconstr Surg, 116(2);613-8; Discussion, 619-20; 2005. 3. Gabbay JS, Eby JB, Kulber DA The midabdominal TRAM flap for breast reconstruction in
morbidly obese patients. Plast Reconstr Surg, 115(3);764-70; 2005 4. Garvey PB, Buchel EW, Pockaj BA, Gray RJ, Samson TD The deep inferior epigastric perforator flap for breast reconstruction in overweight and obese patients. Plast Reconstr Surg, 115(2);447-57; 2005. 5. Moran SL, Serletti JM Outcome comparison between free and pedicled TRAM flap breast reconstruction in the obese patient. Plast Reconstr Surg, 108(7);1954-60; 2001 6. Lin KY, Johns FR, Gibson J, Long M, Drake DB, Moore MM An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol, 8(7);586-91; 2001. 7. Chang DW, Wang B, Robb GL, Reece GP, Miller MJ, Evans GR, Langstein HN, Kroll SS Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg, 105(5);1640-8; 2000 8. Disa JJ, Ad-El DD, Cohen SM, Cordeiro PG, Hidalgo DA The premature removal of tissue expanders in breast
reconstruction. Plast Reconstr Surg, 104(6);1662-5; 1999 9. Paige KT, Bostwick J 3rd, Bried JT, Jones G A comparison of morbidity from bilateral, unipedicled and unilateral, unipdicled TRAM flap breast reconstructions. Plast Reconstr Surg, 101(7);1819-27, 1998



 Évről-évre egyre jelentősebbé válik az internetes álláspiac, hiszen számos offline hirdetési forma szűnt meg az álláskereső portálok térnyerésével. A gördülékeny egymásra találásnak köszönhetően a munkahelyváltás könnyebb, mint valaha. Tudd meg, hogyan!
Évről-évre egyre jelentősebbé válik az internetes álláspiac, hiszen számos offline hirdetési forma szűnt meg az álláskereső portálok térnyerésével. A gördülékeny egymásra találásnak köszönhetően a munkahelyváltás könnyebb, mint valaha. Tudd meg, hogyan!