Please log in to read this in our online viewer!
Please log in to read this in our online viewer!
No comments yet. You can be the first!
What did others read after this?
Content extract
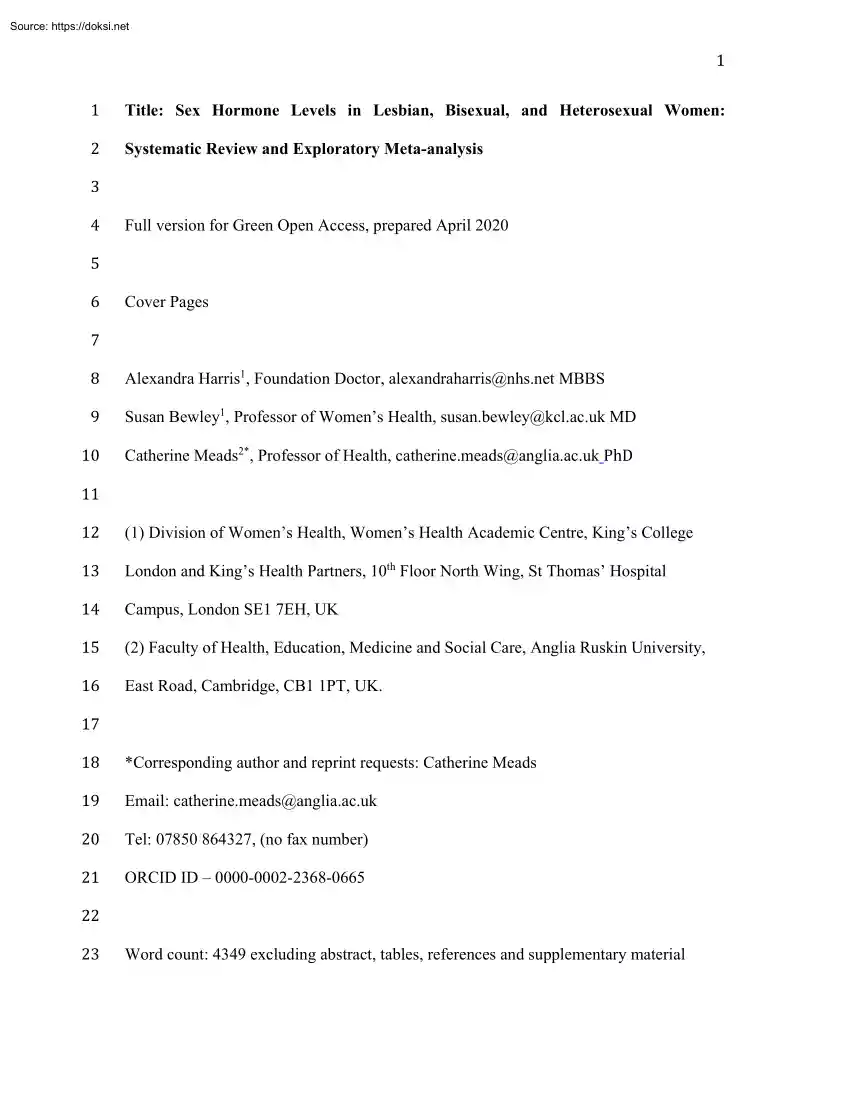
1 1 Title: Sex Hormone Levels in Lesbian, Bisexual, and Heterosexual Women: 2 Systematic Review and Exploratory Meta-analysis 3 4 Full version for Green Open Access, prepared April 2020 5 6 Cover Pages 7 8 Alexandra Harris1, Foundation Doctor, alexandraharris@nhs.net MBBS 10 Catherine Meads2*, Professor of Health, catherine.meads@angliaacuk PhD 12 (1) Division of Women’s Health, Women’s Health Academic Centre, King’s College 14 Campus, London SE1 7EH, UK 16 East Road, Cambridge, CB1 1PT, UK. 18 *Corresponding author and reprint requests: Catherine Meads 20 Tel: 07850 864327, (no fax number) 9 11 13 15 17 Susan Bewley1, Professor of Women’s Health, susan.bewley@kclacuk MD London and King’s Health Partners, 10th Floor North Wing, St Thomas’ Hospital (2) Faculty of Health, Education, Medicine and Social Care, Anglia Ruskin University, 19 Email: catherine.meads@angliaacuk 21 ORCID ID – 0000-0002-2368-0665 23 Word count: 4349 excluding
abstract, tables, references and supplementary material 22 24 25 26 2 Disclosure of Potential Conflicts of Interests: The study arose from an initial project undertaken during a part-funded B.Sc at King’s College London (AH) but was otherwise 27 unfunded. The authors had no financial support for this work 29 in the submitted work in the previous three years and there were no other relationships or 31 that they have no conflict of interest. 33 Ethical Approval: This article does not contain any studies with human participants 35 Research Involving Human Participants and/or Animals: Not applicable as it’s a 37 Informed Consent: Not applicable as it’s a systematic review 28 30 32 There were no financial relationships with any organizations that might have an interest activities that could appear to have influenced the submitted work. The authors declare 34 performed by any of the authors as it’s a systematic review 36 systematic review. 38 39 40 41 42
43 Keywords: lesbian; bisexual women; sex hormones; systematic review; meta-analysis 44 Abstract 46 compared to heterosexual women. We systematically reviewed comparative studies 48 CRD42017072436) and searches conducted in six databases. Any relevant empirical 50 sexual minority women compared to heterosexual women were included, with no 52 conducted in duplicate. Random-effects meta-analyses of hormone levels, using 54 reported results. From 1236 citations, 24 full papers were examined and 14 studies of 56 measured in plasma (n = 9), saliva (n = 4), and urine (n = 2) and included 58 and several other hormones. Most studies were small, biased, and had considerable 45 3 Lesbian and bisexual women may have different levels of sex hormones 47 measuring any sex hormones. A protocol was prospectively registered (PROSPERO - 49 studies published within the last 50 years reporting any circulating sex hormones in 51 language or setting restrictions. Inclusions,
data extraction, and quality assessment were 53 standardized-mean-differences (SMD) were conducted where five or more studies 55 mixed designs included, 12 in women without known ovarian problems. Hormones were 57 androstenedione, luteinizing hormone, estradiol, pregnanediol, progesterone, testosterone, 59 heterogeneity. Few found statistically significant differences between groups All-sample 61 heterosexual women (n = 9; SMD = 0.90; 95% Confidence Interval (CI) 022, 157, I2 = 60 meta-analysis showed increased testosterone in sexual minority women compared to 62 84%). This was the only difference found We conclude that the small amount of 64 sex hormone levels between lesbian, bisexual, and heterosexual women excepting 66 placing any certainty in the findings or their implications. 63 heterogeneous research, from 50 years to date, suggests little discernable difference in 65 possibly higher testosterone. A large-scale primary study would be required before 67
68 INTRODUCTION 70 heterosexual women in prevalence of several physical conditions (Meads et al., 2018; 69 4 Health research in sexual minority women has shown that they differ from 71 Robinson et al., 2017) For example, a systematic review showed higher rates of chronic 73 women compared to heterosexual women, but no significant difference in rates of 75 Another systematic review demonstrated higher rates of asthma but not cardiovascular 77 women compared to heterosexual women (Meads et al., 2018) It is currently unclear if 79 evidence (Meads & Moore, 2013). One study from the US has shown a higher mortality 81 higher incidence, poorer access to treatment, or other factors such as avoidance of 83 illness rates is somewhat puzzling if there were indeed no physiological differences 85 different sex hormone levels. 87 James, 2005; Meyer-Bahlburg, 1979; O’Hanlan, Gordon, & Sullivan, 2018), with no firm 89 though there has been a suggestion that
prenatal testosterone levels may influence life- 72 74 pelvic pain and cervical cancer, and lower rates of uterine cancer in lesbians and bisexual polycystic ovarian syndrome, endometriosis, and fibroids (Robinson et al., 2017) 76 disease, despite higher cardiovascular disease risk profiles in lesbians and bisexual 78 there are higher rates of breast cancer incidence or not, due to lack of good quality 80 rate from breast cancer (Cochran & Mays, 2012), but it is uncertain whether this is due to 82 screening and over-diagnosis of low-grade lesions. Emerging evidence of these different 84 between sexual minority women and heterosexual women. One explanation may lie in 86 Female sexual orientation has been investigated for decades (Balthazart, 2011; 88 conclusions drawn about why women may become heterosexual, bisexual or lesbian, 90 long sexual orientation (Balthazart, 2011). Potential correlations between sex hormones 5 91 and sexual orientation have been
approached in three main ways. There has been 93 differences in hormonal regulation (Downey et al., 1987) A second route has been by 95 in heterosexual and homosexual people (Balthazart, 2011), for example by looking at 97 there has been investigation of activational effects of sex hormones from measurement of 99 Some reviews state that prenatal sex hormones are causally associated with sexual 92 investigation of differences in brain sexual differentiation that may lead to lasting 94 investigating organizational effects of any alteration of the prenatal hormone environment 96 second and fourth finger ratios (2D:4D ratios). Thirdly, and of relevance to this project, 98 their levels in post-pubertal homosexual people (Downey et al., 1987) 100 orientation of “butch” lesbians (James, 2005; O’Hanlan, Gordon, & Sullivan, 2018), but 102 congenital adrenal hyperplasia (Stout et al., 2010) A number of researchers have 101 this seems to be an extrapolation from
findings from research about women with 103 investigated various markers that may be associated with the prenatal hormonal milieu 105 second and fourth finger ratios (2D:4D ratios) (Swift-Gallant et al., 2020), among various 107 discusses differences in genetic and hormonal pathways and whether either may have a 109 hormones in mammalian (including human) sexual differentiation is clear, its role in 104 and sexual orientation, such as handedness (Lalumière, Blanchard, & Zucker, 2000) or 106 other parameters. A more recent extensive review of sexual orientation controversies 108 part to play in causation of sexual orientation (Bailey et al., 2016) While the role of 110 sexual orientation is less clear. 112 has also failed to consider the place of bisexual women. Studies have tended to either 111 113 Historically, much of the research into the biological basis of sexual orientation consider bisexuality as a subset of homosexuality or disregard it entirely.
Therefore, in 6 114 research studies, bisexual women could fall into either homosexual or heterosexual 116 1995). 118 adulthood, but no systematic reviews. An early review by Meyer-Bahlburg (1979) 120 puberty but a third have elevated androgen levels. It is unclear as to how it was discerned 115 117 groups depending on how they were perceived by the researcher (Van Wyk & Geist, There have been several reviews of sex hormone levels and female sexuality in 119 concluded that the majority of female homosexuals have normal sex hormone levels after 121 that “a third of the subjects studied had elevated androgen levels” as many of the included 123 clear. Meyer-Bahlburg also stated that variation in adult androgen levels did not affect 122 papers were on transsexuals not lesbians and the normal levels and cut-off used were not 124 sexual orientation. Subsequent reviews focused more on issues of trying to extrapolate 126 effects of environmental stress (Banks
& Gartrell, 1995). 128 heterosexual women, it is unclear which hormones would be involved, if there is a 130 are two primary sources of sex steroids: ovaries and adrenal glands and the role of each 132 secondary, or confounding, rather than causative, or affect subgroups of sexual minority 134 It could also be that lesbian practices (or other factors) might lead to changes in 125 127 results from mammals to humans (Birke, 1981) or discussed potential confounding If there is a difference in hormone levels between lesbian, bisexual, and 129 hormonal “threshold” which must be met, and if it applies to all (Balthazart, 2011). There 131 may vary. It may also be that any differences in hormones found are incidental, 133 women only, such as those who look or pass as more “masculine.” 135 sex hormone levels. Similarly, higher levels of chronic stress in society might lead to 136 lower average hormone levels, including for sex hormones such as luteinizing
hormone 137 (LH), follicle stimulating hormone (FSH), prolactin, progesterone and testosterone, and 139 This systematic review evaluates all published human research on sex hormone 138 higher levels of estrogen. Most research in this area is on non-human animals 140 levels in sexual minority women compared to heterosexual women. 141 METHOD 143 was lodged with PROSPERO (CRD42017072436) in September 2017. 142 7 This systematic review was conducted according to a prospective protocol which 144 Inclusion Criteria 146 minority women self-described as; lesbian or bisexual, women who described themselves 145 147 Studies were eligible using the following inclusion criteria: (1) Population: sexual as having sex with women (WSW), or having sex with women and men (WSWM); or 148 women co-habiting or married to women, and who were identified as women at birth, and 150 included papers, including (but not limited to) androstenedione, estradiol, luteinizing 152 women or
women self-describing as only having sex with men or married to men; and 154 Study design: any comparative studies including randomized controlled trials, 156 secondary studies with data of interest. Studies had to contain primary data and be peer- 158 restrictions on setting or language. Studies were excluded if: the sexual orientation and/or 149 are not taking exogenous sex hormones. (2) Exposure: any sex hormones as reported in 151 hormone, pregnanediol, progesterone, and testosterone; (3) Comparator: heterosexual 153 who were identified as women at birth, and are not taking exogenous hormones. (4) 155 experimental studies, cohort studies, case-control studies, cross-sectional analyses, or 157 reviewed. Only studies published between 1969 and 2019 were eligible There were no 159 behavior of women were not clear; there was no comparison with heterosexual women; 160 there were no outcomes of interest; or if they were opinions, editorials, conference 162
excluded if all participants were taking exogenous hormones (e.g, transgender women 8 161 abstracts, or case reports. Although not specified in the protocol, studies would have been 163 who were born male and were taking estrogen supplements). 164 Search Strategy, Study Selection and Data Extraction 166 Search terms and appropriate synonyms (as MeSH terms and text words) were developed 168 Nursing Index (Ovid), Cochrane Central (Cochrane Library), Medline (Ovid), Embase 165 167 Searches were conducted by one reviewer (AH) and checked by another (CM). based on population and exposures. Six databases (platforms) were searched - British 169 (Ovid), PsycInfo (Ovid), and Science Citation Index (Web of Science). The same search 171 terms can be found in Online Supplement Appendix 1. Searches were conducted up to 173 were no language restrictions. All titles found by the above search were assessed for 175 were also hand searched to identify any relevant papers not found
by database searching. 177 abstracts may not have mentioned the measurement of relevant sex hormones. If any 179 read and either accepted for the systematic review or rejected based on the above 181 systematic review was carried out by two reviewers (AH, CM). Any disagreements were 170 terms were used for each database but adapted where necessary. A full table of search 172 June 2018, and redone using the same search terms and databases in May 2019. There 174 inclusion and abstracts read. Reference lists of relevant reviews and accepted studies 176 We also checked studies on lesbian health used in other projects because titles and 178 titles and abstracts had relevant information or there was uncertainty, the full study was 180 inclusion and exclusion criteria. Full-text assessment to determine inclusion in the 182 resolved by discussion. A standard form was devised prior to data extraction and quality 183 scoring, based on the content of the papers and the
aims of the review. Data were 185 contacted about data discrepancies. 184 extracted by one reviewer (AH) and checked by another (CM). No authors were 186 Quality Assessments 188 (CM), and reported in the categories of risk of bias, study design issues, and whether the 190 checklist that would be appropriate for all of the studies due to the diverse study designs 192 Data Analysis 194 different hormones measured. Results for women with medical conditions were assessed 196 version 5.3, on hormone levels where five or more studies reported results in a similar 198 women comparator was used. Heterogeneity was assessed using the I2 test, using 200 sample type (blood, saliva, urine), and presence or absence of contraceptive pill use, 202 RESULTS 204 available and were read. Fourteen studies were included in the narrative synthesis and 187 189 191 193 Studies were appraised for selection, performance, attrition, and detection biases study would be representative of
the general population. There is no single validated so a formal quality assessment tool was not used. Results for plasma, saliva, and urinary analyses were tabulated separately by the 195 separately to those without conditions. Meta-analysis was conducted, using RevMan 197 way. Where multiple sexual minority subgroups were present, the same heterosexual 199 established thresholds. Subgroup analysis was performed where relevant, according to 201 inclusion of postmenopausal women, and sample taken in the post-luteal phase. 203 From 1236 citations, 104 abstracts were selected, of which 24 full papers were 9 10 205 nine in the meta-analyses. See Online Supplement Figure 1 (PRISMA flow chart) and 207 Study Characteristics 209 1. Study designs used were case-control (n = 6), cross sectional (n = 6) and cohort (n = 211 all published in English and originated from: USA (n = 6), UK (n = 5), Taiwan (n = 1), 213 four had no details on study funding. Recruitment methods
varied with most studies 215 gynecology outpatient clinic (Agrawal et al., 2004) and one in two fertility clinics (Chen 217 word of mouth, or consecutive patients; and in some studies a combination was used. 206 208 210 Online Supplement Table 1 (excluded studies with reasons). The 14 studies were published between 1970 and 2016, and are detailed in Table 2), see Online Supplement Table 2 (quality assessment of included studies). Studies were 212 Canada (n = 1) and the Netherlands (n = 1). Funding sources were wide ranging, although 214 occurring outside of the healthcare environment (n = 12), but one was performed in a 216 et al., 2014) Participants were recruited by a variety of methods, including advertising, 218 Two early studies gave no recruitment details (Gooren, 1986; Loraine et al., 1970) The 220 (Loraine et al., 1970) to 254 (Agrawal et al, 2004) Participants were all within adult 219 number of sexual minority women included in the primary studies ranged
from 4 221 reproductive age range (15 - 45) except one early study, which included participants up to 222 223 55 years old (Griffiths et al., 1974), without clarification of numbers related to menopausal status. Sexual minority status was determined by self-reporting of: self- 224 identified orientation, history of sexual behavior, and/or feelings of sexual attraction. Five 226 1990; Downey et al., 1987; Gladue, 1991; Juster et al, 2016; Neave, Menaged, & 225 studies also used a numerical scale of sexual orientation or sexual preference (Dancey, 227 Weightman, 1999). Six studies specified a length of time participants must have 11 228 identified as lesbian or bisexual (Chen et al., 2014; Downey et al, 1987; Gartrell, 230 time requirement given was 12 months (Downey et al., 1987; Gartrell, Loriaux, & Chase, 232 1986). In one study, lesbians were divided into subgroups according to sexual history 234 et al., 1999) the sexual minority women participants
were divided into “butch” and 236 2011; Juster et al., 2016), with one grouping them with lesbian women (Juster et al, 238 2011). Heterosexual women were the comparator group in 12 studies, one study used a 229 Loriaux, & Chase, 1977; Gladue, 1991; Gooren, 1986; Smith et al., 2011 The minimum 231 1977) and the maximum was exclusive life-long orientation (Gladue, 1991; Gooren, 233 (primary, intermediate, and secondary lesbians) (Dancey, 1990) and in one study (Singh 235 “femme.” Only two of the 14 studies included bisexual women (Diamond & Wallen, 237 2016) and the other reporting results for bisexual women separately (Diamond & Wallen, 239 comparator population of women who did not identify as lesbian or bisexual (Diamond & 240 Wallen, 2011), and one study used reference ranges from textbooks and results from a 242 In one study, self-reported information and blood test results were examined by a 241 previous study (Griffiths et al., 1974)
243 reproductive endocrinologist (Griffiths et al., 1974) Hormones were measured in plasma 245 hormone results (Juster et al., 2016) Hormones measured included 17-oxosteroids (n = 244 (n = 9), saliva (n = 4), and urine (n = 2), one study reported both plasma and salivary 246 1), androstenedione (n = 5), DHEAS (n = 2), epitestosterone (n = 2), FSH (n = 2), LH (n 247 = 3), estriol (n = 2), estrone (n = 2), estradiol (n = 10), pregnanediol (n = 2), pregnanetriol 249 results for testosterone because one paper reported results separately for “butch” and 248 250 (n = 1), progesterone (n = 4), prolactin (n = 2), and testosterone (n = 15). There were 15 “femme” women (Singh et al., 1999) Timing of hormone sampling was controlled for in 12 251 some studies by time of day (n = 8) (Diamond & Wallen, 2011; Downey et al., 1987; 253 Neave, Menaged, & Weightman, 1999; Singh et al., 1999) and by point in menstrual 255 al., 1987; Gartrell, Loriaux, & Chase,
1977; Gladue, 1991; Gooren, 1986; Griffiths et al, 257 menstrual/endocrine abnormalities (n = 7) (Chen et al. 2014; Downey et al, 1987; 259 Singh et al., 1999; Smith et al, 2011) Current use of hormonal preparations (eg 261 (Juster et al., 2016) and not mentioned in two early studies (Griffiths et al, 1974; Loraine 263 measured in three studies (Agrawal et al., 2004; Chen et al, 2014; Smith et al, 2010) All 252 Gartrell, Loriaux, & Chase, 1977; Gladue, 1991; Juster et al., 2016; Loraine et al, 1970; 254 cycle (n = 9) (Agrawal et al., 2004; Dancey, 1990; Diamond & Wallen, 2011; Downey et 256 1974; Neave, Menaged, & Weightman, 1999). Some studies noted a medical history of 258 Gartrell, Loriaux, & Chase, 1977; Gladue, 1991; Neave, Menaged, & Weightman, 1999; 260 contraceptive pill) was specifically excluded for participants in all studies except one 262 et al., 1970) Hormone levels in polycystic ovarian syndrome (PCOS) patients were 264 of the
participants in Chen et al., (2014) had PCOS but fewer than 10% of the participants 266 hormone levels for women with normal ovaries separately from those with PCO and 268 provided reference ranges for one or more hormone (Chen et al., 2014; Dancey, 1990; 270 presented separately for plasma (n = 9) (see Online Supplement Table 3), saliva (n = 4) 265 in Smith et al., (2010) had PCOS (13/211) The study by Agrawal et al, (2004) gave 267 PCOS, but the results were not reported separately in Smith et al., (2011) Five studies 269 Griffiths et al., 1974; Juster et al, 2016; Smith et al, 2011) Numerical results are 271 (see Online Supplement Table 4), and urine hormones (n = 2) (see Online Supplement 272 273 Table 5). 13 274 Findings in Healthy Women 276 heterosexual women without known ovarian problems, measured in more than one study 278 Loraine et al., 1970) showed significant reductions in sexual minority women compared 280 2), LH (n = 3), estriol (n = 2), and
progesterone (n = 4), and no significant difference in 282 (n = 2), and pregnanediol (n = 2) (see Table 2). There were also no differences seen in the 284 (Griffiths et al., 1974), and prolactin (Agrawal et al, 2004) in women without known 286 lesbians (Singh et al., 1999) showed a significant increase for the “butch” lesbians 288 difference between “femme” lesbians and heterosexual women (of any appearance). 290 ovarian problems were conducted. For testosterone, there was a significant increase in 292 (see fig 1) compared to heterosexual women, but no significant increase in the plasma 294 = 7, SMD = -0.03 (95% CI -024 to +018, I2 = 0%)) or in any subgroup by sampling type 275 Direction of difference in hormone levels in sexual minority women compared to 277 are shown in Table 2. The two early studies measuring estrone (Griffiths et al, 1974; 279 to heterosexual women. There were mixed results in epitestosterone (n = 2), DHEAS (n = 281 levels between
sexual minority and heterosexual women in androstenedione (n = 5), FSH 283 single studies that measured 17-oxosteroids (Griffiths et al., 1974), pregnanetriol 285 ovarian problems. The one study measuring testosterone in “butch” and “femme” 287 compared to “femme” lesbians and compared to heterosexual women, but no significant 289 Exploratory meta-analyses in testosterone and estradiol in women without known 291 293 295 sexual minority women overall (n = 9, SMD = +0.90; 95% CI +022 to +157, I2 = 84%) testosterone subgroup results. For estradiol, there was no significant difference overall (n (see fig 2). 296 Subgroup analysis of the testosterone meta-analysis removing the study using 14 luteal sampling (Dancey, 1990) increased the overall SMD to +1.19 (95% CI +047 to 297 298 +1.91) Subgroup analysis removing the study explicitly including participants using the 299 300 contraceptive pill (Juster et al., 2016) decreased the overall SMD to +063 (95%
CI +008 to +1.18) Adding in results for bisexual women (Dancey, 1990) decreased the overall 301 SMD slightly to +0.82 (95% CI +019 to +145) 303 difference to the overall result. The only study enrolling participants over the age of 50 305 meta-analysis. 302 All of the subgroup analyses for the estrogen meta-analysis made very little 304 (who may have been menopausal) (Griffiths et al., 1974) did not contribute to either 306 Results in Women with Polycystic Ovary Syndrome. 308 2014; Smith et al., 2010) As Smith et al (2011) did not give results for sexual minority 310 women with PCOS, their results are given in the section above. Agrawal et al (2004) 307 Three studies included women with PCOS (Agrawal et al., 2004; Chen et al, 309 women with PCOS separately to those without PCOS, and there were fewer than 10% of 311 gave results separately for women with PCOS and all participants in Chen et al. (2014) 313 lower levels of estradiol in one study (Chen et al., 2014)
but not in the other (Agrawal et 312 had PCOS. For sexual minority women with PCOS, there were statistically significantly 314 al., 2004), and higher levels of testosterone, androstenedione, and free androgen index in 316 heterosexual women. There were no significant differences found in levels of DHEAS 318 2004; Chen et al., 2014), and prolactin (Agrawal et al, 2004) 315 one study (Agrawal et al., 2004), but not in the other (Chen et al, 2014), compared to 317 (Agrawal et al., 2004), FSH (Agrawal et al, 2004; Chen et al, 2014), LH (Agrawal et al, 319 DISCUSSION 15 320 Main Findings 322 minority women. Our findings suggest little discernible difference in plasma hormone 324 testosterone levels, and only when combining blood, saliva and urine results across 326 collection. If there are higher rates of testosterone in sexual minority women, the current 328 testosterone levels may be an incidental finding rather than causative of health 330 Strengths and
Limitations 332 presentation of numerical results, inclusion of global data from a variety of sources, and a 334 changed over time but each study used the same methods for all of their participant 336 study and used standardized mean differences in the meta-analyses, absolute differences 338 cannot be certain that each of the studies measured hormones in the same part of the 340 these differences would cancel each other, but in small sample sizes there may be 321 There has been disappointingly little research into sex hormone levels in sexual 323 levels between sexual minority and heterosexual women except for possibly higher 325 studies which were small with considerable variation in methods of hormonal data 327 evidence is not sufficient to determine whether this is in a subset or not. Also, the 329 differences. There were inconsistent results in women with PCOS 331 Strengths included protocol preregistration in the PROSPERO database, careful 333 search for
any relevant studies from the last 50 years. Methods of hormone assays have 335 groups. Therefore, as we looked for relative differences between groups within each 337 in measurement methods across studies will not impact on the results. However, we 339 menstrual cycle in each participant. Where studies had relatively large samples, hopefully 341 consistent differences because of this. It would be uncertain as to which direction these 342 343 344 345 16 differences would lie. Also, participants in most of the studies were not explicitly asked if they had PCOS or even congenital adrenal hyperplasia (CAH), both of which can affect testosterone levels. Participants in some studies were split into subgroups of sexual minority status, such as primary, intermediate, or secondary lesbians (for definitions see 346 Online Supplement Table 2) (Dancey, 1990) or "butch" and "femme" (Singh, Vidaurri, 348 thereby diluting the main effect of sexual minority vs
heterosexual women. Therefore we 350 testosterone levels found in the all sample meta-analysis would apply to all lesbians and 347 Zambarano, & Dabbs, 1999), with little justification, and results presented separately, 349 cannot tell from the small amount of studies so far whether the slightly higher 351 bisexual women or to a subgroup. It is uncertain as to how any subgroups would be 353 Interpretation 355 minority women. Other studies are consistent with some of the findings, for example 357 “butch” lesbians had higher testosterone levels than their partners who rated themselves 359 Vidaurri, Zambarano, & Dabbs, 1999). However, when combined results for all “butch” 361 suggesting that the relative rather than absolute difference is more important, or that the 363 heterogeneity of findings was of particular importance in the testosterone findings, where 352 354 defined. There have been no recent systematic reviews of sex hormone levels in sexual
356 Pearcey, Docherty, & Dabbs (1996) found that when measured in butch/femme pairs, 358 as more “femme,” which is similar to the findings in one of our included studies (Singh, 360 partners were compared to all “femme” partners, no significant differences were seen, 362 sample size was too small to determine absolute differences in testosterone levels. The 364 there was some statistically significant evidence of a relationship between androgens and 17 365 sexual orientation. However, the problem is that there are a number of endocrine 367 contraceptive or menstrual regulation use), and thus it would be crucial that these 369 study by Singh et al. (1999) participants were not explicitly asked if they had PCOS or 371 syndrome (CAIS), a condition that effectively makes androgen action impossible, 373 endocrine factors that would affect androgen levels is unknown. Similarly, in Smith et al 375 as they made up only 10% of the sample, thus confounding
any relationship between 377 Implications for Policymakers 379 were confirmed, higher rates of conditions associated with higher testosterone levels such 366 conditions that might affect levels of androgens (such as CAH, PCOS, and oral 368 variables are controlled for, which was not consistently the case. In the aforementioned 370 even CAH. They were not asked whether they had congenital androgen insensitivity 372 regardless of androgen levels. Thus, the composition of the sample in relation to 374 (2011), which did include women with PCOS, these results were not presented separately 376 378 testosterone and sexual minority status. If the tentative finding of higher levels of testosterone in sexual minority women 380 as PCOS might be expected to be observed, although a recent systematic review has not 382 currently unclear. Also, finding a difference tells us nothing about the direction of 381 383 demonstrated this (Robinson et al., 2017) Therefore, any
clinical implications remain causality. Testosterone levels in the blood can be raised indirectly by stress and there has 384 been much work around minority stress in sexual minorities (Meyer, 2003). Thus, it is 386 another cause, or merely an incidental finding. More clarity is required before any 385 unclear if our tentative finding of higher testosterone levels is because of minority stress, 387 implications for health in sexual minority women can be discussed. 18 388 Implications for Research 390 women so far and most previous studies have had small sample sizes. In the 40 years 392 Bahlburg (1979) review. There also appears to be very little information on variations of 394 establish sex hormone levels in sexual minority women compared to heterosexual women 389 391 There has been very little research into sex hormone levels in sexual minority since its publication, research seems not to have progressed much further than the Meyer- 393 androgen and
estrogen receptor sensitivity. A large, well conducted study is needed to 395 so that potential influences on the health of sexual minority women can be estimated. 397 an online two group sample size calculator, at 95% CI (alpha of 0.05), beta of 2 and 399 SD 6.27 lesbian, mean 147 heterosexual group), we estimate that a single study which 401 is fewer than in the Forest plot, but much larger than almost all of the included studies. 403 Study of Parents and Children (ALSPAC) study, to investigate links between sex 396 This could also measure variations of androgen and estrogen receptor sensitivity. Using 398 power of 80%, and means and SDs taken from the testosterone Forest plot (mean 17.4, 400 could look at all hormone profiles should have 170 participants, 85 in each group, which 402 It may be possible to use cohort data, for example from the Avon Longitudinal 404 hormone and receptor sensitivity levels and sexual orientation. This large cohort study 406 years,
and collected blood samples at various ages, including at age 24. Regarding PCOS 408 or registry data, which would be feasible if they recorded sexual orientation. An 410 cohabitation status should be routinely recorded as part of data collection in research 405 enrolled participants before birth, recorded adolescents' sexual orientation at age 15 407 and other rarer conditions, some questions can only be answered by case-control studies 409 important implication for future research is that sexual orientation, sexual behavior, and 19 411 studies, alongside medical records, to allow more large scale interpretation of hormone 413 Conclusion 415 sexual minority women and heterosexual women except for possibly higher testosterone 417 finding or its refutation. The paucity of primary studies may relate to a lack of interest, 419 and some on behavior. However, while identity and behavior are overlapping categories, 412 414 416 levels, disease patterns, and
potential confounders including stress levels. Our findings suggest little discernible difference in hormone levels between levels, but a large-scale primary study would be needed to increase the certainty of this 418 lack of funding, or stigmatization of the topic. Some included studies focused on identity 420 they must be distinguished in research by recording and presenting both. 421 422 423 Tables and figures list 424 Figure 1: Random effects subgroup meta-analysis of testosterone levels by sample 426 problem. 428 lesbians and heterosexual women with no known ovarian or endocrine problem 430 Table 2: Hormone levels, measured in more than one study, showing statistically 432 minority women compared to heterosexual women without known ovarian problems 434 Online Supplement 436 Data Extraction Form 20 425 method in lesbians and heterosexual women with no known ovarian or endocrine 427 Figure 2: Random effects subgroup meta-analysis of estradiol levels by
sample method in 429 Table 1: Characteristics of included studies 431 significantly increased (↑), decreased (↓), same levels () or not measured () in sexual 433 435 Search Strategy 437 Online Supplement Table 1: Full Text Excluded Studies with Reasons for Exclusion 439 Online Supplement Table 3: Plasma Hormone Results 441 Online Supplement Table 5: Urine Hormone Results 438 Online Supplement Table 2: Quality Assessment of Studies 440 Online Supplement Table 4: Saliva Hormone Results 442 Online Supplement Figure 1: PRISMA Flow Diagram 443 21 444 445 446 447 448 Figure 1: Random Effects Subgroup Meta-analysis of Testosterone Levels by Sample Method in Sexual Minority and Heterosexual Women with No Known Ovarian or Endocrine Problem. 22 449 450 451 452 453 Figure 2: Random Effects Subgroup Meta-analysis of Estradiol Levels by Sample Method in Sexual Minority and Heterosexual Women with No Known Ovarian or Endocrine Problem. 23 454 Table 1.
Characteristics of Included Studies Author Population Determinatio Comparator Year Recruitment n Recruitment Country of Sexual Orientation Agrawal 2004 UK Chen 2014 Taiwan Lesbian women n=254 Consecutive recruiting of women who attended The London Women’s Clinic and Hallam Medical Centre for ovulation induction between November 2001 and January 2003. Selfidentification of orientation and history of sexual behavior discussed in interviews, Heterosexual women n=364 Recruitment same as lesbian women. Lesbians with PCOS n=8 Recruited by medical history questionnaire at Gynecology Outpatients Department of Taipei Medical University Hospital. Self-reporting and description of sexual history over past 2 years on questionnaire s. Heterosexual women with PCOS n=89 Recruitment same as for lesbian women. Hormones Measured Method (Reference ranges) Plasma Androstenedione DHEAS FSH LH Estradiol Testosterone Age Range (Moderators Controlled for) Age range: 20-45 years old (mean 35.4)
(Timing of venipuncture on early follicular phase, ie days 2-3 of menstrual cycle. No participants had previous exposure to androgens or androgen elevating substances or used hormonal therapy in the last year.) Plasma Fasting: Age range: 20-35 Androstenedione years old FAI (Timing regarding FSH menstrual cycle not LH specified). (No LH/FSH ratio participants were Estradiol taking OCP or experiencing Total testosterone menopausal (Hyperandrogenism: symptoms at time of Conditions Funding Related to Hormones Levels Measured Acne No information BMI Hirsutism Oligo-/ amenorrhea Ovarian volume PCOS Polycystic ovaries Acne BMI Hirsutism Hyperandro genism Oligomennorrhoea PCOS Joint grant from Taipei Medical University and Taipei Medical University Hospital and also by the Ministry of Science and 24 tT elevated and A (>2.4 ng/mL)) Dancey 1990 UK Diamond Lesbians (n=30) separated into 3 categories: Primary lesbians (n=10), intermediate lesbians (n=10), secondary lesbians (n=10)#
Recruitment by response to advertisements: Letters left in women’s clubs, pubs, and bookshops. Adverts in women’s magazines. Women who responded were given letters to give to their female friends. Lesbian women Self-definition as lesbian/ heterosexual. Primary emotional/sex ual attractions fulfilled by women (lesbians) or men (heterosexuals). Heterosexual women n=10 Recruitment same as for lesbians. Plasma Androstenedione Estradiol Progesterone Testosterone Testosterone/proge sterone ratio (Luteal phase testosterone: 0.525nmol/L) venipuncture, or had ever been diagnosed with Cushing’s syndrome, androgen-secreting tumors, or congenital adrenal hyperplasia.) Age range: 21-41 (mean 28.4 ± 496) (Timing of venipuncture on luteal phase, ie days 4-9 after ovulation). No participants were taking hormonal preparations.) Non-lesbian Salivary estradiol Mean age = 30 Technology, Executive Yuan and Taipei Veterans General Hospital. - Grant from the Central Research Fund Committee,
University of London. - Grant from Corroborated by score on SOM questionnaire . Self-reporting 25 2010 USA Downey 1987 USA n=5 Bisexual women n=7 Part of larger longitudinal study to study sexual identity development. Initial sampling at lesbian, gay, and bisexual community events, youth groups, and classes on gender and sexuality issues taught at local colleges and universities in interviews and online diary throughout longitudinal study. Homosexual women n=7 Recruitment by advertisement within a university community. Kinsey scale score based on partner preference of sexual fantasies and behavior and nonbisexual women who either identified as hetero-sexual or did not claim to have a sexual identity. These women had previously identified as lesbian or bisexual at the start of the longitudinal study. n=8 Recruiting the same as for lesbian and bisexual women. Hetero-sexual women n=7 Recruitment same as for homo-sexual women. years. (Timing of sample collection started 9
days after first day of menstrual period and consistent time of day. No participants were pregnant, breast feeding, or taking OCP at the time of sample collection.) Plasma Androstenedione Testosterone Age range: 19-29 (Timing of venipuncture on days 1-3 of menstrual cycle and between 8-9am on each day. Matching National Institutes of Child Health and Human Development. University of Utah Research Committee grant. - BRSG grant of the Research Foundation for Mental Hygiene; USPHS NIMH Research 26 during previous 12 months. Gartrell 1977 USA Homosexual women n=21 Recruitment: referred by local “homophile organizations”. Sexual behavior included only same-sex partners (homosexuals) or opposite sex partners (heterosexuals) for the preceding year. Heterosexual women n=19 No details of recruitment. Plasma Testosterone of homosexual and heterosexual participants according to: age, height, weight, level of education, and whether or not they had a live in partner. No
participants had irregular menstrual cycles, had used OCP in the previous year, or been exposed to diethylstilbestrol prenatally.) Age range homosexual women: 21-35; heterosexual women: 21-33. (Timing of venipuncture on days 1-3 of menstrual cycle and at 8am each day. No participants were taking OCP or had menstrual irregularities.) Scientist Development Award; Research Center Grants - No details 27 Gladue 1991 USA Gooren 1986 Netherland s Lesbians n=16 Recruited using newspaper ads, posters, referrals from friends and previous volunteers Categorized by Kinsey scale using information from questionnaires and interview data. Only included if exclusive lifelong (since puberty) homosexual or heterosexual history. Heterosexual women n=16 Recruitment same as lesbians women. Plasma Estradiol Testosterone (free and total) (Reference range not given but states results are in normal limits.) Age range: lesbians 21-32; heterosexual women: 27-21 (Timing of venipuncture on day 6 of
menstrual cycle and between 1-4pm on one day. No participants used OCP or had known endocrine abnormalities.) - Homosexual women n=6 No details of recruitment Self-reporting of orientation. Lesbians had a life-long history of exclusive or near Heterosexual women n=6 Plasma LH, Estradiol Testosterone Age range: homosexual women: 24-32; heterosexual women: 22-27. (Timing of venipuncture on day - No details of recruitment. Harry Frank Guggenheim Foundation; National Science Foundation Experimental Program to Stimulate Competitive Research; Achieving Science Excellence in North Dakota Project, National Science Foundation Research Experiences for Undergraduates Program. No details 28 exclusive homosexual orientation Griffiths 1974 Lesbian women: n=36 UK Juster 2016 Recruited through lesbian organizations Selfidentification as lesbian and member of lesbian organization “Normal” subjects from a previous study for estradiol, estriol and estrone n=not given Lesbian
women N=8 Bisexual women Selfidentification of orientation Heterosexual women n=20 3-5 of menstrual cycle between 8.3010am No participants had used hormonal preparations in 15 months before the study began.) Urinary Lesbians age 17-oxosteroids range: 22-55 (Comparator Epitestosterone population of an Estradiol, Estriol “appropriate age Estrone Prenanediol group” Timing of sampling in relation Pregnanetriol to menstrual cycle Testosterone (Reference ranges: was noted for lesbian subjects. pregnanediol: 6.2Comparator 15.6 (luteal) pregnanetriol: 0.3population samples taken at 8.9 “appropriate stage” 17-Oxosteroids: 17.4-559 of menstrual cycle. (µmol/24)5 Use of OCP was epitestosterone: 6.9- noted and taken 61.8 into account when reporting results.) testosterone: 3.5413 (nmol/24hr)) Salivary fasting Age range: 18-45 estradiol (Timing of sample Progesterone collection between - Endowment fund of St. Thomas Hospital Blood pressure BMI Canadian Institutes of Health 29
Canada n=13 Recruited as part of a broader research program. Separate advertisements according to sexual orientation. Loraine 1970 Lesbians n=4 No information on recruitment. by responding to one of three separate adverts asking for heterosexual, bisexual or lesbian participants and in telephone consultation. Corroborated using Klein Sexual Orientation Scale. Self-reporting of orientation and sexual behavior. Neave 1999 Lesbian women n=14 UK Recruited through homophile Self-reporting and score on questionnaire derived from UK Recruitment the same as for lesbian and bisexual women. Testosterone (Saliva) Plasma fasting DHEAS (DHEAS range: 1.2104 µmol/l) 12 noon and 7pm each day, phase of menstrual cycle not stated. Use of oral contraceptive use and phase of menstrual cycle was considered in analysis.) Cholesterol level Insulin level Triglyceride level Research. RP Juster Doctoral Scholarship from The Institute of Aging of Canadian Institutes of Health Research. Heterosexual
women n=not given Members of lab the staff who did not admit to homosexual inclinations. Heterosexual women n=14 Recruited from Urinary Epitestosterone FSH, LH Estradiol Estriol, Estrone Pregnanediol Testosterone Lesbians age range: 20-23 (age not given for controls). (Samples taken throughout menstrual cycle.) - No information Salivary Testosterone Age range: Lesbians: 19-43 (mean 26); Heterosexual - University of Northumbria Small Research 30 Singh 1999 USA organizations and friendship networks. sell scale of sexual orientation. Northumbria University student population and in the community matched to lesbian women in terms of education level and age. Lesbian women (n=33) separated into “butch” (n=17) and “femme” (n=16) categories according to score on personal history questionnaire. Recruited by “Snowball”/networkin g technique to find friends/acquaintance s of researchers who then recruited more participants by word Selfidentification as lesbian or
heterosexual Heterosexual women n=11 Same as for lesbian women Salivary Fasting: Testosterone women: 20-43 (mean 31), (Timing of sample collection according to menstrual cycle and consistent time of day. No participants were taking hormone influencing drugs (including OCP), had abnormal menstrual cycles, or had medical conditions affecting hormone level.) Age range: 25-45 (Timing of sample collection at 7-9am each day, phase of menstrual cycle not stated. No participants were taking OCP or had known ovarian problem.) Grants Scheme. BMI Age at menarche National Science Foundation Grant 31 Smith 2010 USA 455 456 of mouth. Lesbian women n=114 Recruitment using participants of the ESTHER Project who agreed to be contacted about further studies. Recruited to original study by local advertisement and community events Self-identified as nonheterosexual and reported only or primarily having emotional, physical, and romantic attraction towards women within the past 5 years or were
in relationships with only or primarily women within the past 5 years. Heterosexual women n=97 Self-identified as heterosexual/ straight and only had male partners since the age of 18. Plasma Fasting: Androstenedione Testosterone (Biochemical hyperandrogensism: tT ≥3.4ng/mL and A >2.4ng/mL) Age range: 35-45 (Venipuncture phase of menstrual cycle not stated. No participants were using OCP at time of venipuncture, displayed menopausal symptoms, or had a previous diagnosis of Cushing’s syndrome, androgen secreting tumors, congenital adrenal hyperplasia.) Acne BMI Hirsutism Infertility PCOS Oligomenorrhea ESTHER Project funded by National Lung, Blood and Heart Association. PCOS study funded by ESTHER Project, Lambda Foundation and Lesbian Health Fund (Gay and Lesbian Medical Association). Key: #Primary lesbians: Never had heterosexual experiences or interest, scored less than 20 on the heterosexual component of SOM. Intermediate 457 lesbians: Prior heterosexual experience or
interest and scored less than 20 on the heterosexual part of the SOM. Secondary Lesbians: Prior 459 Hormones: A: androstenedione; DHEAS: dehydroepiandrosterone sulphate; E2: estradiol; FAI: free androgen index (testosterone/ sex hormone 458 heterosexual experience or interest and scored more than 20 on the heterosexual part of the SOM (Dancey et al, 1990). 32 460 binding globulin x100); FSH: follicle stimulating hormone; L2: luteinizing hormone; P: progesterone; T: testosterone; fT: free testosterone, tT: total 462 Abbreviations: ESTHER – BMI – body mass index, BRSG – Biomedical Research support Grant, Epidemiologic Study of Health Risk. Nmol – 464 micromoles, USPHS NIMH – United States Public Health Service National Institute for Mental Health 461 testosterone. 463 nanomoles, OCP – oral contraceptive pill, PCO – polycystic ovaries, PCOS – polycystic ovary syndrome, SOM - sexual orientation method, µmol – 465 33 466 467 468 469 Table 2.
Hormone Levels, Showing Statistically Significantly Increased (↑), Decreased (↓), Same Levels (), or Not Measured () in Sexual Minority Women Compared to Heterosexual Women Without Known Ovarian Problems Author, date Androstene- DHEAS Epitestost- Estriol Estrone EstraFSH LH Pregnane- Progest- Testostdione erone diol diol erone erone Agrawal 2004 Dancey 1990p Dancey 1990i Dancey 1990s Diamond 2010 Downey 1987 Gartrell 1977 ↑ Gladue 1991 Gooren 1986 Griffiths 1974 ↓ ↑ Juster 2016 ↑ ↑ Loraine 1970 ↑ ↓ ↓ ↓ ↑ ↑ Neave 1999 Singh 1999 ↑ (“butch”) Singh 1999 (“femme”) Smith 2010 ACKNOWLEDGMENTS: We thank Miss Melanie Davies for comments on an earlier draft. We thank the anonymous peer reviewers and Editor on Chief for their comments. 34 REFERENCES 35 Agrawal, R., Sharma, S, Bekir, J,
Conway, G, Bailey, J, Balen, A H, & Prelevic, G (2004). Prevalence of polycystic ovaries and polycystic ovary syndrome in lesbian women compared with heterosexual women. Fertility & Sterility, 82(5), 1352-1357 doi:10.1016/jfertnstert200404041 Bailey, J. M, Vasey, P L, Diamond, L M, Breedlove, S M, Vilain, E, & Epprecht, M (2016). Sexual Orientation, Controversy, and Science Psychological Science in the Public Interest, 17(2), 45-101. doi:101177/1529100616637616 Balthazart, J. (2011) Minireview: Hormones and human sexual orientation Endocrinology, 152(8), 2937-2947. doi:101210/en2011-0277 Banks, A., & Gartrell, N K (1995) Hormones and sexual orientation: a questionable link Journal of Homosexuality, 28(3-4), 247-268. doi:101300/J082v28n03 04 Birke, L. I (1981) Is homosexuality hormonally determined? Journal of Homosexuality, 6(4), 35-49. Chen, C. H, Wang, P H, Hsieh, M T, Tzeng, C R, Wu, Y H, Lee, C S, Chu, H-Y, & Chang, H. Y (2014) Sexual orientations of women
with polycystic ovary syndrome: clinical observation in Taiwan. Taiwan Journal of Obstetrics and Gynecology, 53(4), 542-546 doi:10.1016/jtjog201409002 Cochran, S. D, & Mays, V M (2012) Risk of breast cancer mortality among women 36 cohabiting with same sex partners: findings from the National Health Interview Survey, 1997-2003. Journal of Womens Health, 21(5), 528-533 doi:101089/jwh20113134 Dancey, C. P (1990) Sexual orientation in women: an investigation of hormonal and personality variables. Biological Psychology, 30(3), 251-264 Diamond, L. M, & Wallen, K (2011) Sexual minority women's sexual motivation around the time of ovulation. Archives of Sexual Behavior, 40(2), 237-246 doi:101007/s10508-0109631-2 Downey, J., Ehrhardt, A A, Schiffman, M, Dyrenfurth, I, & Becker, J (1987) Sex hormones in lesbian and heterosexual women. Hormones and Behavior, 21(3), 347-357 Gartrell, N. K, Loriaux, D L, & Chase, T N (1977) Plasma testosterone in homosexual and
heterosexual women. American Journal of Psychiatry, 134(10), 1117-1118 doi:10.1176/ajp134101117 Gladue, B. A (1991) Aggressive Behavioral Characteristics, Hormones and Sexual Orientation in Men and Women. Aggressive Behavior, 17, 313-326 Gooren, L. (1986) The neuroendocrine response of luteinizing hormone to estrogen administration in heterosexual, homosexual, and transsexual subjects. Journal of Clinical Endocrinology and Metabolism, 63(3), 583-588. doi:101210/jcem-63-3-583 Griffiths, P. D, Merry, J, Browning, M C, Eisinger, A J, Huntsman, R G, Lord, E J, 37 Whitehouse, R. H (1974) Homosexual women: an endocrine and psychological study Journal of Endocrinology, 63(3), 549-556 James, W. H (2005) Biological and psychosocial determinants of male and female human sexual orientation. Journal of Biosocial Science, 37(5), 555-567 doi:10.1017/S0021932004007059 Juster, R. P, Almeida, D, Cardoso, C, Raymond, C, Johnson, P J, Pfaus, J G, Lupien, S. J (2016) Gonads and strife: Sex
hormones vary according to sexual orientation for women and stress indices for both sexes. Psychoneuroendocrinology, 72, 119-130 doi:10.1016/jpsyneuen201606011 Lalumière M.L, Blanchard R, & Zucker KJ (2000) Sexual orientation and handedness in men and women: a meta-analysis. Psychological Bulletin, 126(4), 575-92 Loraine, J. A, Ismail, A A, Adamopoulos, D A, & Dove, G A (1970) Endocrine function in male and female homosexuals. British Medical Journal, 4(5732), 406-409 Meads, C., Martin, A, Grierson, J, & Varney, J (2018) Systematic review and metaanalysis of diabetes mellitus, cardiovascular and respiratory condition epidemiology in sexual minority women. BMJ Open, 8(4), e020776 doi:101136/bmjopen-2017-020776 Meads, C., & Moore, D (2013) Breast cancer in lesbians and bisexual women: systematic 38 review of incidence, prevalence and risk studies. BMC Public Health, 13, 1127 doi:10.1186/1471-2458-13-1127 Meyer-Bahlburg, H. F (1979) Sex hormones and female
homosexuality: a critical examination. Archives of Sexual Behavior, 8(2), 101-119 Meyer, I. H (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129(5), 674697 doi:101037/0033-29091295674 Neave, N., Menaged, M, & Weightman, D R (1999) Sex differences in cognition: the role of testosterone and sexual orientation. Brain and Cognition, 41(3), 245-262 doi:10.1006/brcg19991125 O'Hanlan, K. A, Gordon, J C, & Sullivan, M W (2018) Biological origins of sexual orientation and gender identity: Impact on health. Gynecologic Oncology, 149(1), 33-42 doi:10.1016/jygyno201711014 Pearcey, S. M, Docherty, K J, & Dabbs, J M, Jr (1996) Testosterone and sex role identification in lesbian couples. Physiology & Behavior, 60(3), 1033-1035 Robinson, K., Galloway, K Y, Bewley, S, & Meads, C (2017) Lesbian and bisexual women's gynaecological conditions: a systematic
review and exploratory meta-analysis. BJOG, 124(3), 381-392. doi:101111/1471-052814414 39 Singh, D., Vidaurri, M, Zambarano, R J, & Dabbs, J M, Jr (1999) Lesbian erotic role identification: behavioral, morphological, and hormonal correlates. Journal of Personality and Social Psychology, 76(6), 1035-1049. Smith, H. A, Markovic, N, Matthews, A K, Danielson, M E, Kalro, B N, Youk, A O, & Talbott, E. O (2011) A comparison of polycystic ovary syndrome and related factors between lesbian and heterosexual women. Womens Health Issues, 21(3), 191-198 doi:10.1016/jwhi201011001 Stout, S. A, Litvak, M, Robbins, N M, & Sandberg, D E (2010) Congenital adrenal hyperplasia: classification of studies employing psychological endpoints. International Journal of Pediatric Endocrinology, 2010, 191520. doi:101155/2010/191520 Swift-Gallant, A., Johnson, B A, Di Rita, V, & Breedlove, S B (2020) Through a glass, darkly: Human digit ratios reflect prenatal androgens, imperfectly. Hormones
and Behavior, 120, 104686. doiorg/101016/jyhbeh2020104686 Van Wyk, P. H, & Geist, C S (1995) Biology of bisexuality: critique and observations Journal of Homosexuality, 28(3-4), 357-373. doi:101300/J082v28n03 11 40 Online supplement material Sex Hormone Levels in Lesbian, Bisexual, and Heterosexual Women: Systematic Review & Exploratory Meta-analysis Online Supplement Contents: Search Terms Used and Search Strategy for At Least One Database Data Extraction Form Table 1 - Full Text Excluded Studies with Reasons for Exclusion Table 2 - Quality Assessment of Included Studies Table 3 – Plasma Hormone Results Table 4 - Saliva Hormone Results Table 5 - Urine Hormone Results Figure 1 – PRISMA Flow Diagram 41 Search Terms Used and Search Strategy for At Least One Database Search Terms Used on First and Second Round of Literature Searching (Lesbian OR Bisexual OR Homosexual) AND Hormone OR ?estrogen OR Androgen OR Testosterone OR Progesterone OR LH OR FSH OR GnRH OR
ACTH OR CRH OR Activin OR Inhibin Literature Searching Customized to Each Database. Database Customization of Search Search Type Used Pubmed Term “Homosexual” not included Title and Abstract as clearly covered in MeSH terms CENTRAL - Titles, Abstracts, Key Words EMBASE - Abstract British Nursing “?” omitted from ?estrogen as Index search engine did not Abstract understand function Web of Science - Topic Psych Info - Abstract Data Extraction Form Name of Study Authors Year of Publication Study Type Setting Method of Recruitment Funding Country Timescale Aim of Study Exposure Outcome Size of Study Populations Age Range Inclusion Criteria Exclusion Criteria Comparator Population Hormones Measured Method Timing of Hormone Measurement Hormone Related Conditions Measured Additional Tests/Investigations Determination of Sexual Orientation Additional Diagnostic Criteria Hormone 42 Study Demographics Population Description Comments Lesbian Bisexual
Heterosexual Methods Description Comments Fasting Menstrual Diurnal Unit Hormonal Data Lesbian Bisexual 43 Hormone Reference Ranges Condition/Variable Measured Statistical Analysis Notes Additional Data Unit Lesbian Bisexual Online Supplement Table 1: Excluded Studies with Reasons for Exclusion Author, Year Baker et al. 2002 Juster et al. 2015 Title Testosterone, Alcohol and Civil and Rough Conflict Resolution Strategies in Lesbian Couples Oral Contraceptives, Androgens and the Sexuality of Young Women: II. The Role of Androgens Is Homosexuality Hormonally Determined? PCOS in Lesbian and Heterosexual Women Treated with Artificial Donor Insemination. Testing the Affiliation Hypothesis of Homoerotic Motivation in Humans: The Effects of Progesterone and Priming Neuroendocrine Response to Estrogen and Sexual Orientation Significance of Androgen Levels in the Aetiology and Treatment of Homosexuality Sexual Orientation Modulates Endocrine Stress Reactivity Loraine et al.
1971 Patterns of Hormone Excretion in Male and Female Homosexuals Pearcey et al. 1995 Testosterone and Sex Role Identification in Lesbian Couples Bancroft et al. 1991 Birke 2012 De Sutter et al. 2008 Fleischman et al. 2014 Gladue et al. 1984 James et al. 1977 44 Reason for Exclusion No heterosexual control group or normal reference range to use as control Hormonal data only for women using OCP or not. No data grouped by sexual orientation Review article Hormone levels not included in final analysis as too many patients data was missing Progesterone levels not separated according to sexual orientation No data on lesbian or bisexual women Study on males only No data on sex hormone levels only how sex hormones affect cortisol Further discussion of an earlier study already being used in this SR No heterosexual control group or normal reference range to use as control Online Supplement Table 2: Plasma Hormone Results Study Method Hormone Year Timing (Units) Agrawal et
Venipuncture on day 2 or 3 of al. Chen et al. 2014 Populations and results given as mean and (SD) Lesbians menstrual cycle. 2004 45 P value Statistical Significance Test L vs. H1 Two tailed t Heterosexuals NO PCO PCOS NO PCO PCOS PCO PCOS (n=51) (n=107) (n=97) (n=248) (n=65) (n=51) A (nmol/L) - 7.032 12.82 - 6.092 8.132 NS <0.001* DHEAS (µg/ml) 3.7 (08) 6.1 (1) 7.4 (16) 4.9 (09) 4.9 (08) 6 (1.2) NS NS E2 (pmol/l) 162 (32) 169 (36) 170 (45) 162 (35) 156 (28) 169 (43) NS NS FAI - 3.752 12.032 - 2.52 5.632 <0.01* <0.001* FSH (IU/l) 7.7 (14) 6.9 (12) 5.4 (09) 7.9 (16) 6.5 (13) 6 (0.7) NS NS LH (IU/l) 4.5 (05) 4.8 (04) 7.8 (09) 4.4 (05) 4.8 (03) 7.3 (10) NS NS Prolactin (mIU/L) 412 (56) 364 (40) 376 (40) 340 (43) 365 (34) 362 (34) NS NS T (nmol/L) - 2.032 3.442 - 1.722 2.662 <0.05* <0.05* tests, MannWhitney U tests (details not given as to which tests used for each hormone)
Lesbians with PCOS (n=8) Heterosexuals with PCOS (n=89) L vs. H Unpaired t A (ng/ml) 2.4 (10) 2.4 (15) 0.936 test E2 (pmol/l) 59.1 (134) 129.7 (1512) <0.001* FAI 0.08 (004) 0.07 (011) 0.790 FSH (IU/l) 5.7 (13) 5.6 (21) 0.874 Fasting venipuncture Dancey LH/FSH ratio 2.20 (065) 2.90 (180) 0.242 LH (IU/l) 12.7 (51) 15.1 (81) 0.422 Prolactin (ng/mL) 21.2 (133) 13.3 (63) 0.141 T (ng/ml) 0.34 (013) 0.41 (024) 0.432 PL (n=10) Venipuncture during luteal IL (n=10) SL (n=10) H (n=10) ovulation) of menstrual cycle. A (nmol/L) 8.29 (359) 7.69 (237) 9.38 (372) 9.52 (418) 0.69 Ovulation kits used to E2 (pmol/L) 408.44 (27503) 306.8 (1282) 463.7 (20004) 424.5 (17516) 0.31 determine point in cycle. P (nmol/L) 23.7 (1511) 28.5 (2337) 25.2 (1956) 29.9 (2908) 0.98 T (nmol/L) 2.24 (058) 1.98 (088) 2.58 (135) 2.56 (130) 0.58 T/P (ratio) 0.17 (017) 0.17 (021) 0.53 (075) 0.34 (047) 0.90 Downey et Venipuncture between 8 and
al. 9am on 1st, 2nd and 3rd days of menstrual period1. Average of 1987 Gartrell et al. Lesbians (n=7) Heterosexuals (n=7) L vs. H A (ng/100ml) 112 (19) 124 (36) NS T (ng/100ml) 32 (12) 32 (5) NS Lesbians (n=21) Heterosexuals(n=19) L vs. H Details not 36 (11) 26 (7) <0.001* given t tests 3 specimens. Venipuncture at 8am of days 1, 2 and 3 of menstrual 1977 ANOVA all 4 groups phase (day 4-9 after 1990 ANOVA run across 46 cycle3. Average of three samples taken. T (ng/100mL) Gladue 1991 Gooren et al. Venipuncture on day 6 of No details Not given No details LB vs. H ANCOVA 41.4 (149) 36.9 (92) and 4pm. Two samples taken fT (pg/ml) 1.75 (07) 2.31 (12) one hour apart. tT (ng/dl) 47 (18) 37 (10) Lesbians (n=6) Heterosexuals (n=6) E2 (pg/ml) 36 (9) 34 (10) LH (mIU/ml) 5.2 (12) 5.0 (10) T (ng/ml) 0.29 (011) 0.32 (01) Fasting venipuncture between LB Heterosexual 8am and 11am (n=20) (n=20) 7.34 (064) 5.58 (037) 0.027*
Lesbians (n=114) Heterosexuals (n=97) L vs. H Wilcoxon Venipuncture during days 3-6 2016 2010 Not given E2 (pg/ml) 1986 Smith et al. Heterosexuals (n=16) menstrual cycle between 1 of menstrual cycle Juster et al. Lesbians (n=16) 47 DHEAS µmol/l Analysis carried out on blood stored from previous study A (ng/ml) 1.63 (median) 1.51 (median) 0.079 rank-sum (fasting venipuncture). T (ng/ml) 1.69 (median) 1.52 (median) 0.069 tests Key: Hormones: A: androstenedione; DHEAS: dehydroepiandrosterone sulphate; E2: estradiol; FAI: free androgen index (testosterone/SHBGx100); FSH: follicle stimulating hormone; L2: luteinising hormone; P: progesterone; T: testosterone; fT: free testosterone, tT: total testosterone. Populations: H: heterosexual women; IL: intermediate lesbians; L: lesbians; LB: lesbian and bisexual women; PL: primary lesbians; SL: secondary lesbians. Dancey et al (1990 defines these as Primary – lesbians with no heterosexual interest or experience, and
scored less than 20 on the Sexual Orientation Method questionnaire, Intermediate - lesbians with prior heterosexual interest or experience, and scored less than 20 on the Sexual Orientation Method 48 questionnaire, Secondary - lesbians with prior heterosexual interest or experience and scored more than 20 on the Sexual Orientation Method questionnaire. Conditions: NO: normal ovaries; PCO: polycystic ovaries; PCOS: polycystic ovary syndrome. Statistics: ANOVA: analysis of variance; ANCOVA: analysis of covariance. NS: not significant 1 Statistical significance was analysed in all hormones for which levels are given All differences in women with normal ovaries were not significant. 2Data extracted from graphs; (med): value is median NOT mean 3Day 1 defined as 8am which occurred within 24 hours of menstrual onset. *Statistically significant result: 49 Online Supplement Table 3: Saliva Hormone Results Study Method Hormone Year Timing (unit) Diamond Daily saliva samples for
10 days at 2010 the same time each day starting on E2 (pg/ml) Population and results given as mean and (SD) L (n=5) B (n=7) NLB (n=8) 1.9 (05) 1.9 (07) 2.2 (19) P value Statistical Significance test Not given No details ANCOVA day 9 of menstrual cycle. Juster 2016 LB (n=20) H (n=20) LB vs. H E2 (pg/ml) 4.33 (042)1 4.58 (458)1 NS P (pg/ml) 122.92 (1667)1 66.67 (1667)1 <0.05* T (pg/ml) 64.44 (444)1 48.89 (444)1 0.006* Saliva samples produced at same Lesbians Heterosexuals Homosexual men/women vs. stage in menstrual cycle at 10am- (n=13) (n=12) heterosexual men + women 37.50 (833) 1 22.22 (556)1 0.06 Saliva sample taken between 12pm and 7pm. Neave 1999 12pm or 2pm-4pm over 2 months. Singh 1999 T (pg/ml) Fasting saliva sample between 7 Butch L Femme L H and 9am (n=17) (n=16) (n=11) 4.1 (17) 2.5 (08) 2.3 (09) T (ng/ml) BuL vs. FL BuL vs. H FL vs. H <0.001* <0.001* 0.99 ANOVA ANOVA Hormones: E2: estradiol; P:
progesterone; T: testosterone. Populations: B: bisexuals; BuL: butch lesbians; FL: femme lesbians; H: heterosexual women; L: lesbian; LB: lesbians and bisexuals; NLB: no longer lesbian or bisexual identity. Statistics: ANOVA: analysis of variance; ANCOVA: analysis of covariance; NS: not significant 1Data extracted from graphs. *Statistically significant result. 50 Online Supplement Table 4 - Urine Hormone Results Study Method Hormone Year Timing (Units) Griffiths Urine et al. sample timing in 1974 Population and results given as mean and (SD) P value Significance Lesbians (n=36) Reference Range 17-O (μmol/24hr) 28.8 (69-743) 17.4-5591 E1 (nmol/24hr) 8.1 (0-483) Onset of menses:14.8-258; Ovulation peak: 406-1144; Luteal: relation to Not given No details 36.9-8492 menstrual E2 (nmol/24hr) 4.4 (0-165) Onset of menses: 0-11; Ovulation peak: 14.7-514; Luteal: 147-3672 cycle was E3 (nmol/24hr) 26.6 (0-1183) Onset of menses: 0-51.9; Ovulation peak:
45-1868; 277-29412 noted. Pgn2 (μmol/24hr) 9.7 (28-300) Follicular: <3.12; Luteal: 62-1561 Pgn3 (μmol/24hr) 1.8 (006-39) 0.3-891 T (nmol/24hr) 33.7 (0-913) 3.5-4133 eT (nmol/24hr) 33.0 (0-1024) 6.9-6183 Loraine 48 hour L1 L2 L3 L4 L Mean4 H et al. pools of (n=1) (n=1) (n=1) (n=1) (n=4) (n=not L vs. H No details given) urine 1970 Test produced E1 (μmol/24hr) 6.7 (29) 7.1 (45) 1.5 (29) 1.1 (22) 4.1 (31) 9.5 (48) All comparisons <0.05-0001* throughou E2 (μmol/24hr) 3.9 (17) 3.7 (32) 1.1 (24) 0.5 (05) 2.3 (20) 3.5 (24) L1,L2 p=NS, L3,L4 p<0.001* . t cycle. E3 (μmol/24hr) 11.0 (6) 6.5 (44) 13.6 (97) 3.8 (22) 8.7 (56) 9.7 (65) Results L1,L3 p=NS, L2 p<0.01, L4 p<0.001 given as FSH (IU/24hr) 9.0 (73) 10.4 (131) 3.6 (20) 6.0 (49) 7.3 (68) 7.3 (18) L1,L2,L4 p=NS L3 p<0.001 value per LH (IU/24hr) 12.4 (223) 26.0 (232) 37.1 (312) 30.7 (295) 26.6 (265) 11.1 (41) L1 p=NS, L2, L4 p <0.05,
24 hours. L3 p<0.01 Pgn2 (mg/24hr) 1.4 (07) 2.0 (15) 0.5 (05) 1.0 (10) 1.2 (09) 1.2 (17) L1,L3,L4 p=NS, L2 p<0.001 T (μmol/24hr) 11 (1.8) 17.3 (26) 16.0 (25) 30.0 (53) 18.6 (31) 7.3 (43) All comparisons <0.05-0001* eT (μmol/24hr) 9.2 (65) 18.2 (75) 14.1 (105) 14.1 (102) 13.9 (87) 8.9 (48) L1,L3,L4 p=NS, L2 p<0.001 Key: 17-O: 17-oxosteroids; E1: estrone; E2: estradiol; E3: estriol; FSH: follicle stimulating hormone; L2: luteinising hormone; Pgn2: pregnanediol; Pgn3: pregnanetriol; T: testosterone; eT: epitestosterone. S: Significant 1Textbook values from “Hormone Assays and their Clinical Applications (Loraine and Bell 1966).2: “Normal” appears to heavily imply heterosexual (or at least not lesbian) but this is not explicit (Brown 1955) 3Textbook values taken from “Gas Chromatographic Determination of Normal Steroids” (Inguilla et al, 1976). 4Individual means given for each lesbian participant (n=4), mean calculated in Microsoft Excel
during this systematic review for comparative purposes, values given to one decimal place as in study. *Statistically significant result. 51 52 Online Supplement Table 5 - Quality Assessment of Included Studies Study Study Selection Biases Performance Design Biases Agrawal 2004 Cohort Study Consecutive private clinic sample where SMW attending for different reasons to heterosexual women (single and partnered) and partners of SMW. Possibility of misclassification of single women As participants from the different groups attending for different reasons, clinical treatment of each group was different. Attrition Biases Detection Biases Chen 2014 Cross sectional analysis Clinic sample. Unclear if consecutive or not. All have PCOS Not reported Hormone assays similar in all groups. Blinding unclear. Dancey 1990 Case-Control Volunteer sample from community. Paid £12 plus travel expenses – this may have biased volunteering. Unclear if SMW and heterosexual women attending
clinic for the same reason None reported Hormone assays similar in all groups. Blinding unclear. Diamond 2010 Cohort Study Subsample of a larger cohort study investigating sexual identity development. Paid $60 – this may have biased volunteering. None reported The first 10 blood assays from each group were used, possibly introducing bias as later ones discarded There had been 33 participants but 13 gave incomplete data. Downey 1987 Case-Control Volunteer sample from university community. None reported Not reported Gartrell 1977 Case-Control None reported Not reported Gladue 1991 Cross-sectional Study None reported Not reported Gooren 1986 Case-Control Referred sample from ‘homophile organisations’. Unclear where heterosexual sample from. Undergraduate sample volunteering in return for research credits. Possibility of misclassification of sexual orientation. Recruitment method not reported. Hormone assays similar in both groups. Assays done blind to group.
Hormone assays similar in both groups. Blinding unclear. Hormone assays similar in both groups. Blinding unclear. None reported Not reported Not reported Hormone assays similar in all groups. Blinding unclear. Results not given separately for the separate groups. Hormone assays similar in all groups. Blinding unclear. Hormone assays Comment Pathologising of SMW by suggesting 80% have a problem (PCO) whereas the medical condition is PCOS – 38% SMW. No ethics permission statement Excluded second control group without PCOS as no indication of sexual orientation. Unusual separation into ‘primary’, ‘intermediate’ and ‘secondary’ lesbians. Bisexual group excluded as too few. Heteronormative classification of ‘gave up lesbian/bisexual identity’ No ethics permission statement No ethics permission statement No ethics permission statement No ethics permission statement - Study Study Design Selection Biases Performance Biases Attrition Biases Griffiths 1974
Cross-Sectional analysis Lesbians from membership of a lesbian organisation. Comparator was a group of ‘like-aged mothers of a sample of normal children’. Subsample from a larger study, recruitment method not reported. Paid $50 CAD – this may have biased volunteering. Lesbian recruitment method not reported. Controls were members of scientific and technical staff. Possibility of misclassification of sexual orientation. Lesbian volunteers from ‘homophile organisations and friendship networks’ Controls were university students and non-university participants. Recruitment through snowballing or networking via friends and acquaintances of the researchers. Comparator group not sampled at the same time as the lesbian group None reported There were 42 lesbian volunteers but only 36 provided hormone samples Not reported Juster 2016 Cross-sectional analysis Loraine 1970 Case-control study None reported Neave 1999 Case-Control study Singh 1999 Cross-Sectional Analysis
Smith 2010 Cross-Sectional Analysis Subsample from a larger study. Community volunteer sample. Study investigating PCOS, diagnosed blind to sexual orientation. Detection Biases Comment 53 similar in both groups. Blinding unclear. Basal hormone assay levels used only Normal values used for comparator. No ethics permission statement Hormone assay similar in both groups. Blinding unclear. Absolute values for testosterone, estradiol and progesterone not reported. Not reported Lesbian assay results not averaged. No ethics permission statement None reported Testosterone not measured in 2 controls. - None reported Not reported Hormone assay similar in both groups. Blinding unclear. Testosterone levels estimated from graphs. Hormone assay similar in both groups. Blinding unclear. None reported Not reported Hormone assay similar in both groups. Blinding unclear. SMW ‘butch’ and ‘femme’ categories. Study 2 used only. No ethics permission statement Since more women
in the lesbian group had PCOS (7.9%) than in the heterosexual group (4.1%) the mean testosterone levels will be higher in the lesbian group. 54 1 9 10 11 17 18 23 24 Online Supplement Figure 1 – PRISMA Flow Diagram 2 3 Citations Citations 4 identified from identified from reference lists 5 database 6 N=9 searches 7 N=1227 8 Abstracts read in full N=104 12 13 14 15 16 Full texts read in full N=24 19 20 21 22 Included in systematic review N=14 Included in meta-analysis N=9 Citations excluded from title as irrelevant N=1123 Citations excluded from abstract N=71 Studies excluded N=10 (see Table)
abstract, tables, references and supplementary material 22 24 25 26 2 Disclosure of Potential Conflicts of Interests: The study arose from an initial project undertaken during a part-funded B.Sc at King’s College London (AH) but was otherwise 27 unfunded. The authors had no financial support for this work 29 in the submitted work in the previous three years and there were no other relationships or 31 that they have no conflict of interest. 33 Ethical Approval: This article does not contain any studies with human participants 35 Research Involving Human Participants and/or Animals: Not applicable as it’s a 37 Informed Consent: Not applicable as it’s a systematic review 28 30 32 There were no financial relationships with any organizations that might have an interest activities that could appear to have influenced the submitted work. The authors declare 34 performed by any of the authors as it’s a systematic review 36 systematic review. 38 39 40 41 42
43 Keywords: lesbian; bisexual women; sex hormones; systematic review; meta-analysis 44 Abstract 46 compared to heterosexual women. We systematically reviewed comparative studies 48 CRD42017072436) and searches conducted in six databases. Any relevant empirical 50 sexual minority women compared to heterosexual women were included, with no 52 conducted in duplicate. Random-effects meta-analyses of hormone levels, using 54 reported results. From 1236 citations, 24 full papers were examined and 14 studies of 56 measured in plasma (n = 9), saliva (n = 4), and urine (n = 2) and included 58 and several other hormones. Most studies were small, biased, and had considerable 45 3 Lesbian and bisexual women may have different levels of sex hormones 47 measuring any sex hormones. A protocol was prospectively registered (PROSPERO - 49 studies published within the last 50 years reporting any circulating sex hormones in 51 language or setting restrictions. Inclusions,
data extraction, and quality assessment were 53 standardized-mean-differences (SMD) were conducted where five or more studies 55 mixed designs included, 12 in women without known ovarian problems. Hormones were 57 androstenedione, luteinizing hormone, estradiol, pregnanediol, progesterone, testosterone, 59 heterogeneity. Few found statistically significant differences between groups All-sample 61 heterosexual women (n = 9; SMD = 0.90; 95% Confidence Interval (CI) 022, 157, I2 = 60 meta-analysis showed increased testosterone in sexual minority women compared to 62 84%). This was the only difference found We conclude that the small amount of 64 sex hormone levels between lesbian, bisexual, and heterosexual women excepting 66 placing any certainty in the findings or their implications. 63 heterogeneous research, from 50 years to date, suggests little discernable difference in 65 possibly higher testosterone. A large-scale primary study would be required before 67
68 INTRODUCTION 70 heterosexual women in prevalence of several physical conditions (Meads et al., 2018; 69 4 Health research in sexual minority women has shown that they differ from 71 Robinson et al., 2017) For example, a systematic review showed higher rates of chronic 73 women compared to heterosexual women, but no significant difference in rates of 75 Another systematic review demonstrated higher rates of asthma but not cardiovascular 77 women compared to heterosexual women (Meads et al., 2018) It is currently unclear if 79 evidence (Meads & Moore, 2013). One study from the US has shown a higher mortality 81 higher incidence, poorer access to treatment, or other factors such as avoidance of 83 illness rates is somewhat puzzling if there were indeed no physiological differences 85 different sex hormone levels. 87 James, 2005; Meyer-Bahlburg, 1979; O’Hanlan, Gordon, & Sullivan, 2018), with no firm 89 though there has been a suggestion that
prenatal testosterone levels may influence life- 72 74 pelvic pain and cervical cancer, and lower rates of uterine cancer in lesbians and bisexual polycystic ovarian syndrome, endometriosis, and fibroids (Robinson et al., 2017) 76 disease, despite higher cardiovascular disease risk profiles in lesbians and bisexual 78 there are higher rates of breast cancer incidence or not, due to lack of good quality 80 rate from breast cancer (Cochran & Mays, 2012), but it is uncertain whether this is due to 82 screening and over-diagnosis of low-grade lesions. Emerging evidence of these different 84 between sexual minority women and heterosexual women. One explanation may lie in 86 Female sexual orientation has been investigated for decades (Balthazart, 2011; 88 conclusions drawn about why women may become heterosexual, bisexual or lesbian, 90 long sexual orientation (Balthazart, 2011). Potential correlations between sex hormones 5 91 and sexual orientation have been
approached in three main ways. There has been 93 differences in hormonal regulation (Downey et al., 1987) A second route has been by 95 in heterosexual and homosexual people (Balthazart, 2011), for example by looking at 97 there has been investigation of activational effects of sex hormones from measurement of 99 Some reviews state that prenatal sex hormones are causally associated with sexual 92 investigation of differences in brain sexual differentiation that may lead to lasting 94 investigating organizational effects of any alteration of the prenatal hormone environment 96 second and fourth finger ratios (2D:4D ratios). Thirdly, and of relevance to this project, 98 their levels in post-pubertal homosexual people (Downey et al., 1987) 100 orientation of “butch” lesbians (James, 2005; O’Hanlan, Gordon, & Sullivan, 2018), but 102 congenital adrenal hyperplasia (Stout et al., 2010) A number of researchers have 101 this seems to be an extrapolation from
findings from research about women with 103 investigated various markers that may be associated with the prenatal hormonal milieu 105 second and fourth finger ratios (2D:4D ratios) (Swift-Gallant et al., 2020), among various 107 discusses differences in genetic and hormonal pathways and whether either may have a 109 hormones in mammalian (including human) sexual differentiation is clear, its role in 104 and sexual orientation, such as handedness (Lalumière, Blanchard, & Zucker, 2000) or 106 other parameters. A more recent extensive review of sexual orientation controversies 108 part to play in causation of sexual orientation (Bailey et al., 2016) While the role of 110 sexual orientation is less clear. 112 has also failed to consider the place of bisexual women. Studies have tended to either 111 113 Historically, much of the research into the biological basis of sexual orientation consider bisexuality as a subset of homosexuality or disregard it entirely.
Therefore, in 6 114 research studies, bisexual women could fall into either homosexual or heterosexual 116 1995). 118 adulthood, but no systematic reviews. An early review by Meyer-Bahlburg (1979) 120 puberty but a third have elevated androgen levels. It is unclear as to how it was discerned 115 117 groups depending on how they were perceived by the researcher (Van Wyk & Geist, There have been several reviews of sex hormone levels and female sexuality in 119 concluded that the majority of female homosexuals have normal sex hormone levels after 121 that “a third of the subjects studied had elevated androgen levels” as many of the included 123 clear. Meyer-Bahlburg also stated that variation in adult androgen levels did not affect 122 papers were on transsexuals not lesbians and the normal levels and cut-off used were not 124 sexual orientation. Subsequent reviews focused more on issues of trying to extrapolate 126 effects of environmental stress (Banks
& Gartrell, 1995). 128 heterosexual women, it is unclear which hormones would be involved, if there is a 130 are two primary sources of sex steroids: ovaries and adrenal glands and the role of each 132 secondary, or confounding, rather than causative, or affect subgroups of sexual minority 134 It could also be that lesbian practices (or other factors) might lead to changes in 125 127 results from mammals to humans (Birke, 1981) or discussed potential confounding If there is a difference in hormone levels between lesbian, bisexual, and 129 hormonal “threshold” which must be met, and if it applies to all (Balthazart, 2011). There 131 may vary. It may also be that any differences in hormones found are incidental, 133 women only, such as those who look or pass as more “masculine.” 135 sex hormone levels. Similarly, higher levels of chronic stress in society might lead to 136 lower average hormone levels, including for sex hormones such as luteinizing
hormone 137 (LH), follicle stimulating hormone (FSH), prolactin, progesterone and testosterone, and 139 This systematic review evaluates all published human research on sex hormone 138 higher levels of estrogen. Most research in this area is on non-human animals 140 levels in sexual minority women compared to heterosexual women. 141 METHOD 143 was lodged with PROSPERO (CRD42017072436) in September 2017. 142 7 This systematic review was conducted according to a prospective protocol which 144 Inclusion Criteria 146 minority women self-described as; lesbian or bisexual, women who described themselves 145 147 Studies were eligible using the following inclusion criteria: (1) Population: sexual as having sex with women (WSW), or having sex with women and men (WSWM); or 148 women co-habiting or married to women, and who were identified as women at birth, and 150 included papers, including (but not limited to) androstenedione, estradiol, luteinizing 152 women or
women self-describing as only having sex with men or married to men; and 154 Study design: any comparative studies including randomized controlled trials, 156 secondary studies with data of interest. Studies had to contain primary data and be peer- 158 restrictions on setting or language. Studies were excluded if: the sexual orientation and/or 149 are not taking exogenous sex hormones. (2) Exposure: any sex hormones as reported in 151 hormone, pregnanediol, progesterone, and testosterone; (3) Comparator: heterosexual 153 who were identified as women at birth, and are not taking exogenous hormones. (4) 155 experimental studies, cohort studies, case-control studies, cross-sectional analyses, or 157 reviewed. Only studies published between 1969 and 2019 were eligible There were no 159 behavior of women were not clear; there was no comparison with heterosexual women; 160 there were no outcomes of interest; or if they were opinions, editorials, conference 162
excluded if all participants were taking exogenous hormones (e.g, transgender women 8 161 abstracts, or case reports. Although not specified in the protocol, studies would have been 163 who were born male and were taking estrogen supplements). 164 Search Strategy, Study Selection and Data Extraction 166 Search terms and appropriate synonyms (as MeSH terms and text words) were developed 168 Nursing Index (Ovid), Cochrane Central (Cochrane Library), Medline (Ovid), Embase 165 167 Searches were conducted by one reviewer (AH) and checked by another (CM). based on population and exposures. Six databases (platforms) were searched - British 169 (Ovid), PsycInfo (Ovid), and Science Citation Index (Web of Science). The same search 171 terms can be found in Online Supplement Appendix 1. Searches were conducted up to 173 were no language restrictions. All titles found by the above search were assessed for 175 were also hand searched to identify any relevant papers not found
by database searching. 177 abstracts may not have mentioned the measurement of relevant sex hormones. If any 179 read and either accepted for the systematic review or rejected based on the above 181 systematic review was carried out by two reviewers (AH, CM). Any disagreements were 170 terms were used for each database but adapted where necessary. A full table of search 172 June 2018, and redone using the same search terms and databases in May 2019. There 174 inclusion and abstracts read. Reference lists of relevant reviews and accepted studies 176 We also checked studies on lesbian health used in other projects because titles and 178 titles and abstracts had relevant information or there was uncertainty, the full study was 180 inclusion and exclusion criteria. Full-text assessment to determine inclusion in the 182 resolved by discussion. A standard form was devised prior to data extraction and quality 183 scoring, based on the content of the papers and the
aims of the review. Data were 185 contacted about data discrepancies. 184 extracted by one reviewer (AH) and checked by another (CM). No authors were 186 Quality Assessments 188 (CM), and reported in the categories of risk of bias, study design issues, and whether the 190 checklist that would be appropriate for all of the studies due to the diverse study designs 192 Data Analysis 194 different hormones measured. Results for women with medical conditions were assessed 196 version 5.3, on hormone levels where five or more studies reported results in a similar 198 women comparator was used. Heterogeneity was assessed using the I2 test, using 200 sample type (blood, saliva, urine), and presence or absence of contraceptive pill use, 202 RESULTS 204 available and were read. Fourteen studies were included in the narrative synthesis and 187 189 191 193 Studies were appraised for selection, performance, attrition, and detection biases study would be representative of
the general population. There is no single validated so a formal quality assessment tool was not used. Results for plasma, saliva, and urinary analyses were tabulated separately by the 195 separately to those without conditions. Meta-analysis was conducted, using RevMan 197 way. Where multiple sexual minority subgroups were present, the same heterosexual 199 established thresholds. Subgroup analysis was performed where relevant, according to 201 inclusion of postmenopausal women, and sample taken in the post-luteal phase. 203 From 1236 citations, 104 abstracts were selected, of which 24 full papers were 9 10 205 nine in the meta-analyses. See Online Supplement Figure 1 (PRISMA flow chart) and 207 Study Characteristics 209 1. Study designs used were case-control (n = 6), cross sectional (n = 6) and cohort (n = 211 all published in English and originated from: USA (n = 6), UK (n = 5), Taiwan (n = 1), 213 four had no details on study funding. Recruitment methods
varied with most studies 215 gynecology outpatient clinic (Agrawal et al., 2004) and one in two fertility clinics (Chen 217 word of mouth, or consecutive patients; and in some studies a combination was used. 206 208 210 Online Supplement Table 1 (excluded studies with reasons). The 14 studies were published between 1970 and 2016, and are detailed in Table 2), see Online Supplement Table 2 (quality assessment of included studies). Studies were 212 Canada (n = 1) and the Netherlands (n = 1). Funding sources were wide ranging, although 214 occurring outside of the healthcare environment (n = 12), but one was performed in a 216 et al., 2014) Participants were recruited by a variety of methods, including advertising, 218 Two early studies gave no recruitment details (Gooren, 1986; Loraine et al., 1970) The 220 (Loraine et al., 1970) to 254 (Agrawal et al, 2004) Participants were all within adult 219 number of sexual minority women included in the primary studies ranged
from 4 221 reproductive age range (15 - 45) except one early study, which included participants up to 222 223 55 years old (Griffiths et al., 1974), without clarification of numbers related to menopausal status. Sexual minority status was determined by self-reporting of: self- 224 identified orientation, history of sexual behavior, and/or feelings of sexual attraction. Five 226 1990; Downey et al., 1987; Gladue, 1991; Juster et al, 2016; Neave, Menaged, & 225 studies also used a numerical scale of sexual orientation or sexual preference (Dancey, 227 Weightman, 1999). Six studies specified a length of time participants must have 11 228 identified as lesbian or bisexual (Chen et al., 2014; Downey et al, 1987; Gartrell, 230 time requirement given was 12 months (Downey et al., 1987; Gartrell, Loriaux, & Chase, 232 1986). In one study, lesbians were divided into subgroups according to sexual history 234 et al., 1999) the sexual minority women participants
were divided into “butch” and 236 2011; Juster et al., 2016), with one grouping them with lesbian women (Juster et al, 238 2011). Heterosexual women were the comparator group in 12 studies, one study used a 229 Loriaux, & Chase, 1977; Gladue, 1991; Gooren, 1986; Smith et al., 2011 The minimum 231 1977) and the maximum was exclusive life-long orientation (Gladue, 1991; Gooren, 233 (primary, intermediate, and secondary lesbians) (Dancey, 1990) and in one study (Singh 235 “femme.” Only two of the 14 studies included bisexual women (Diamond & Wallen, 237 2016) and the other reporting results for bisexual women separately (Diamond & Wallen, 239 comparator population of women who did not identify as lesbian or bisexual (Diamond & 240 Wallen, 2011), and one study used reference ranges from textbooks and results from a 242 In one study, self-reported information and blood test results were examined by a 241 previous study (Griffiths et al., 1974)
243 reproductive endocrinologist (Griffiths et al., 1974) Hormones were measured in plasma 245 hormone results (Juster et al., 2016) Hormones measured included 17-oxosteroids (n = 244 (n = 9), saliva (n = 4), and urine (n = 2), one study reported both plasma and salivary 246 1), androstenedione (n = 5), DHEAS (n = 2), epitestosterone (n = 2), FSH (n = 2), LH (n 247 = 3), estriol (n = 2), estrone (n = 2), estradiol (n = 10), pregnanediol (n = 2), pregnanetriol 249 results for testosterone because one paper reported results separately for “butch” and 248 250 (n = 1), progesterone (n = 4), prolactin (n = 2), and testosterone (n = 15). There were 15 “femme” women (Singh et al., 1999) Timing of hormone sampling was controlled for in 12 251 some studies by time of day (n = 8) (Diamond & Wallen, 2011; Downey et al., 1987; 253 Neave, Menaged, & Weightman, 1999; Singh et al., 1999) and by point in menstrual 255 al., 1987; Gartrell, Loriaux, & Chase,
1977; Gladue, 1991; Gooren, 1986; Griffiths et al, 257 menstrual/endocrine abnormalities (n = 7) (Chen et al. 2014; Downey et al, 1987; 259 Singh et al., 1999; Smith et al, 2011) Current use of hormonal preparations (eg 261 (Juster et al., 2016) and not mentioned in two early studies (Griffiths et al, 1974; Loraine 263 measured in three studies (Agrawal et al., 2004; Chen et al, 2014; Smith et al, 2010) All 252 Gartrell, Loriaux, & Chase, 1977; Gladue, 1991; Juster et al., 2016; Loraine et al, 1970; 254 cycle (n = 9) (Agrawal et al., 2004; Dancey, 1990; Diamond & Wallen, 2011; Downey et 256 1974; Neave, Menaged, & Weightman, 1999). Some studies noted a medical history of 258 Gartrell, Loriaux, & Chase, 1977; Gladue, 1991; Neave, Menaged, & Weightman, 1999; 260 contraceptive pill) was specifically excluded for participants in all studies except one 262 et al., 1970) Hormone levels in polycystic ovarian syndrome (PCOS) patients were 264 of the
participants in Chen et al., (2014) had PCOS but fewer than 10% of the participants 266 hormone levels for women with normal ovaries separately from those with PCO and 268 provided reference ranges for one or more hormone (Chen et al., 2014; Dancey, 1990; 270 presented separately for plasma (n = 9) (see Online Supplement Table 3), saliva (n = 4) 265 in Smith et al., (2010) had PCOS (13/211) The study by Agrawal et al, (2004) gave 267 PCOS, but the results were not reported separately in Smith et al., (2011) Five studies 269 Griffiths et al., 1974; Juster et al, 2016; Smith et al, 2011) Numerical results are 271 (see Online Supplement Table 4), and urine hormones (n = 2) (see Online Supplement 272 273 Table 5). 13 274 Findings in Healthy Women 276 heterosexual women without known ovarian problems, measured in more than one study 278 Loraine et al., 1970) showed significant reductions in sexual minority women compared 280 2), LH (n = 3), estriol (n = 2), and
progesterone (n = 4), and no significant difference in 282 (n = 2), and pregnanediol (n = 2) (see Table 2). There were also no differences seen in the 284 (Griffiths et al., 1974), and prolactin (Agrawal et al, 2004) in women without known 286 lesbians (Singh et al., 1999) showed a significant increase for the “butch” lesbians 288 difference between “femme” lesbians and heterosexual women (of any appearance). 290 ovarian problems were conducted. For testosterone, there was a significant increase in 292 (see fig 1) compared to heterosexual women, but no significant increase in the plasma 294 = 7, SMD = -0.03 (95% CI -024 to +018, I2 = 0%)) or in any subgroup by sampling type 275 Direction of difference in hormone levels in sexual minority women compared to 277 are shown in Table 2. The two early studies measuring estrone (Griffiths et al, 1974; 279 to heterosexual women. There were mixed results in epitestosterone (n = 2), DHEAS (n = 281 levels between
sexual minority and heterosexual women in androstenedione (n = 5), FSH 283 single studies that measured 17-oxosteroids (Griffiths et al., 1974), pregnanetriol 285 ovarian problems. The one study measuring testosterone in “butch” and “femme” 287 compared to “femme” lesbians and compared to heterosexual women, but no significant 289 Exploratory meta-analyses in testosterone and estradiol in women without known 291 293 295 sexual minority women overall (n = 9, SMD = +0.90; 95% CI +022 to +157, I2 = 84%) testosterone subgroup results. For estradiol, there was no significant difference overall (n (see fig 2). 296 Subgroup analysis of the testosterone meta-analysis removing the study using 14 luteal sampling (Dancey, 1990) increased the overall SMD to +1.19 (95% CI +047 to 297 298 +1.91) Subgroup analysis removing the study explicitly including participants using the 299 300 contraceptive pill (Juster et al., 2016) decreased the overall SMD to +063 (95%
CI +008 to +1.18) Adding in results for bisexual women (Dancey, 1990) decreased the overall 301 SMD slightly to +0.82 (95% CI +019 to +145) 303 difference to the overall result. The only study enrolling participants over the age of 50 305 meta-analysis. 302 All of the subgroup analyses for the estrogen meta-analysis made very little 304 (who may have been menopausal) (Griffiths et al., 1974) did not contribute to either 306 Results in Women with Polycystic Ovary Syndrome. 308 2014; Smith et al., 2010) As Smith et al (2011) did not give results for sexual minority 310 women with PCOS, their results are given in the section above. Agrawal et al (2004) 307 Three studies included women with PCOS (Agrawal et al., 2004; Chen et al, 309 women with PCOS separately to those without PCOS, and there were fewer than 10% of 311 gave results separately for women with PCOS and all participants in Chen et al. (2014) 313 lower levels of estradiol in one study (Chen et al., 2014)
but not in the other (Agrawal et 312 had PCOS. For sexual minority women with PCOS, there were statistically significantly 314 al., 2004), and higher levels of testosterone, androstenedione, and free androgen index in 316 heterosexual women. There were no significant differences found in levels of DHEAS 318 2004; Chen et al., 2014), and prolactin (Agrawal et al, 2004) 315 one study (Agrawal et al., 2004), but not in the other (Chen et al, 2014), compared to 317 (Agrawal et al., 2004), FSH (Agrawal et al, 2004; Chen et al, 2014), LH (Agrawal et al, 319 DISCUSSION 15 320 Main Findings 322 minority women. Our findings suggest little discernible difference in plasma hormone 324 testosterone levels, and only when combining blood, saliva and urine results across 326 collection. If there are higher rates of testosterone in sexual minority women, the current 328 testosterone levels may be an incidental finding rather than causative of health 330 Strengths and
Limitations 332 presentation of numerical results, inclusion of global data from a variety of sources, and a 334 changed over time but each study used the same methods for all of their participant 336 study and used standardized mean differences in the meta-analyses, absolute differences 338 cannot be certain that each of the studies measured hormones in the same part of the 340 these differences would cancel each other, but in small sample sizes there may be 321 There has been disappointingly little research into sex hormone levels in sexual 323 levels between sexual minority and heterosexual women except for possibly higher 325 studies which were small with considerable variation in methods of hormonal data 327 evidence is not sufficient to determine whether this is in a subset or not. Also, the 329 differences. There were inconsistent results in women with PCOS 331 Strengths included protocol preregistration in the PROSPERO database, careful 333 search for
any relevant studies from the last 50 years. Methods of hormone assays have 335 groups. Therefore, as we looked for relative differences between groups within each 337 in measurement methods across studies will not impact on the results. However, we 339 menstrual cycle in each participant. Where studies had relatively large samples, hopefully 341 consistent differences because of this. It would be uncertain as to which direction these 342 343 344 345 16 differences would lie. Also, participants in most of the studies were not explicitly asked if they had PCOS or even congenital adrenal hyperplasia (CAH), both of which can affect testosterone levels. Participants in some studies were split into subgroups of sexual minority status, such as primary, intermediate, or secondary lesbians (for definitions see 346 Online Supplement Table 2) (Dancey, 1990) or "butch" and "femme" (Singh, Vidaurri, 348 thereby diluting the main effect of sexual minority vs
heterosexual women. Therefore we 350 testosterone levels found in the all sample meta-analysis would apply to all lesbians and 347 Zambarano, & Dabbs, 1999), with little justification, and results presented separately, 349 cannot tell from the small amount of studies so far whether the slightly higher 351 bisexual women or to a subgroup. It is uncertain as to how any subgroups would be 353 Interpretation 355 minority women. Other studies are consistent with some of the findings, for example 357 “butch” lesbians had higher testosterone levels than their partners who rated themselves 359 Vidaurri, Zambarano, & Dabbs, 1999). However, when combined results for all “butch” 361 suggesting that the relative rather than absolute difference is more important, or that the 363 heterogeneity of findings was of particular importance in the testosterone findings, where 352 354 defined. There have been no recent systematic reviews of sex hormone levels in sexual
356 Pearcey, Docherty, & Dabbs (1996) found that when measured in butch/femme pairs, 358 as more “femme,” which is similar to the findings in one of our included studies (Singh, 360 partners were compared to all “femme” partners, no significant differences were seen, 362 sample size was too small to determine absolute differences in testosterone levels. The 364 there was some statistically significant evidence of a relationship between androgens and 17 365 sexual orientation. However, the problem is that there are a number of endocrine 367 contraceptive or menstrual regulation use), and thus it would be crucial that these 369 study by Singh et al. (1999) participants were not explicitly asked if they had PCOS or 371 syndrome (CAIS), a condition that effectively makes androgen action impossible, 373 endocrine factors that would affect androgen levels is unknown. Similarly, in Smith et al 375 as they made up only 10% of the sample, thus confounding
any relationship between 377 Implications for Policymakers 379 were confirmed, higher rates of conditions associated with higher testosterone levels such 366 conditions that might affect levels of androgens (such as CAH, PCOS, and oral 368 variables are controlled for, which was not consistently the case. In the aforementioned 370 even CAH. They were not asked whether they had congenital androgen insensitivity 372 regardless of androgen levels. Thus, the composition of the sample in relation to 374 (2011), which did include women with PCOS, these results were not presented separately 376 378 testosterone and sexual minority status. If the tentative finding of higher levels of testosterone in sexual minority women 380 as PCOS might be expected to be observed, although a recent systematic review has not 382 currently unclear. Also, finding a difference tells us nothing about the direction of 381 383 demonstrated this (Robinson et al., 2017) Therefore, any
clinical implications remain causality. Testosterone levels in the blood can be raised indirectly by stress and there has 384 been much work around minority stress in sexual minorities (Meyer, 2003). Thus, it is 386 another cause, or merely an incidental finding. More clarity is required before any 385 unclear if our tentative finding of higher testosterone levels is because of minority stress, 387 implications for health in sexual minority women can be discussed. 18 388 Implications for Research 390 women so far and most previous studies have had small sample sizes. In the 40 years 392 Bahlburg (1979) review. There also appears to be very little information on variations of 394 establish sex hormone levels in sexual minority women compared to heterosexual women 389 391 There has been very little research into sex hormone levels in sexual minority since its publication, research seems not to have progressed much further than the Meyer- 393 androgen and
estrogen receptor sensitivity. A large, well conducted study is needed to 395 so that potential influences on the health of sexual minority women can be estimated. 397 an online two group sample size calculator, at 95% CI (alpha of 0.05), beta of 2 and 399 SD 6.27 lesbian, mean 147 heterosexual group), we estimate that a single study which 401 is fewer than in the Forest plot, but much larger than almost all of the included studies. 403 Study of Parents and Children (ALSPAC) study, to investigate links between sex 396 This could also measure variations of androgen and estrogen receptor sensitivity. Using 398 power of 80%, and means and SDs taken from the testosterone Forest plot (mean 17.4, 400 could look at all hormone profiles should have 170 participants, 85 in each group, which 402 It may be possible to use cohort data, for example from the Avon Longitudinal 404 hormone and receptor sensitivity levels and sexual orientation. This large cohort study 406 years,
and collected blood samples at various ages, including at age 24. Regarding PCOS 408 or registry data, which would be feasible if they recorded sexual orientation. An 410 cohabitation status should be routinely recorded as part of data collection in research 405 enrolled participants before birth, recorded adolescents' sexual orientation at age 15 407 and other rarer conditions, some questions can only be answered by case-control studies 409 important implication for future research is that sexual orientation, sexual behavior, and 19 411 studies, alongside medical records, to allow more large scale interpretation of hormone 413 Conclusion 415 sexual minority women and heterosexual women except for possibly higher testosterone 417 finding or its refutation. The paucity of primary studies may relate to a lack of interest, 419 and some on behavior. However, while identity and behavior are overlapping categories, 412 414 416 levels, disease patterns, and
potential confounders including stress levels. Our findings suggest little discernible difference in hormone levels between levels, but a large-scale primary study would be needed to increase the certainty of this 418 lack of funding, or stigmatization of the topic. Some included studies focused on identity 420 they must be distinguished in research by recording and presenting both. 421 422 423 Tables and figures list 424 Figure 1: Random effects subgroup meta-analysis of testosterone levels by sample 426 problem. 428 lesbians and heterosexual women with no known ovarian or endocrine problem 430 Table 2: Hormone levels, measured in more than one study, showing statistically 432 minority women compared to heterosexual women without known ovarian problems 434 Online Supplement 436 Data Extraction Form 20 425 method in lesbians and heterosexual women with no known ovarian or endocrine 427 Figure 2: Random effects subgroup meta-analysis of estradiol levels by
sample method in 429 Table 1: Characteristics of included studies 431 significantly increased (↑), decreased (↓), same levels () or not measured () in sexual 433 435 Search Strategy 437 Online Supplement Table 1: Full Text Excluded Studies with Reasons for Exclusion 439 Online Supplement Table 3: Plasma Hormone Results 441 Online Supplement Table 5: Urine Hormone Results 438 Online Supplement Table 2: Quality Assessment of Studies 440 Online Supplement Table 4: Saliva Hormone Results 442 Online Supplement Figure 1: PRISMA Flow Diagram 443 21 444 445 446 447 448 Figure 1: Random Effects Subgroup Meta-analysis of Testosterone Levels by Sample Method in Sexual Minority and Heterosexual Women with No Known Ovarian or Endocrine Problem. 22 449 450 451 452 453 Figure 2: Random Effects Subgroup Meta-analysis of Estradiol Levels by Sample Method in Sexual Minority and Heterosexual Women with No Known Ovarian or Endocrine Problem. 23 454 Table 1.
Characteristics of Included Studies Author Population Determinatio Comparator Year Recruitment n Recruitment Country of Sexual Orientation Agrawal 2004 UK Chen 2014 Taiwan Lesbian women n=254 Consecutive recruiting of women who attended The London Women’s Clinic and Hallam Medical Centre for ovulation induction between November 2001 and January 2003. Selfidentification of orientation and history of sexual behavior discussed in interviews, Heterosexual women n=364 Recruitment same as lesbian women. Lesbians with PCOS n=8 Recruited by medical history questionnaire at Gynecology Outpatients Department of Taipei Medical University Hospital. Self-reporting and description of sexual history over past 2 years on questionnaire s. Heterosexual women with PCOS n=89 Recruitment same as for lesbian women. Hormones Measured Method (Reference ranges) Plasma Androstenedione DHEAS FSH LH Estradiol Testosterone Age Range (Moderators Controlled for) Age range: 20-45 years old (mean 35.4)
(Timing of venipuncture on early follicular phase, ie days 2-3 of menstrual cycle. No participants had previous exposure to androgens or androgen elevating substances or used hormonal therapy in the last year.) Plasma Fasting: Age range: 20-35 Androstenedione years old FAI (Timing regarding FSH menstrual cycle not LH specified). (No LH/FSH ratio participants were Estradiol taking OCP or experiencing Total testosterone menopausal (Hyperandrogenism: symptoms at time of Conditions Funding Related to Hormones Levels Measured Acne No information BMI Hirsutism Oligo-/ amenorrhea Ovarian volume PCOS Polycystic ovaries Acne BMI Hirsutism Hyperandro genism Oligomennorrhoea PCOS Joint grant from Taipei Medical University and Taipei Medical University Hospital and also by the Ministry of Science and 24 tT elevated and A (>2.4 ng/mL)) Dancey 1990 UK Diamond Lesbians (n=30) separated into 3 categories: Primary lesbians (n=10), intermediate lesbians (n=10), secondary lesbians (n=10)#
Recruitment by response to advertisements: Letters left in women’s clubs, pubs, and bookshops. Adverts in women’s magazines. Women who responded were given letters to give to their female friends. Lesbian women Self-definition as lesbian/ heterosexual. Primary emotional/sex ual attractions fulfilled by women (lesbians) or men (heterosexuals). Heterosexual women n=10 Recruitment same as for lesbians. Plasma Androstenedione Estradiol Progesterone Testosterone Testosterone/proge sterone ratio (Luteal phase testosterone: 0.525nmol/L) venipuncture, or had ever been diagnosed with Cushing’s syndrome, androgen-secreting tumors, or congenital adrenal hyperplasia.) Age range: 21-41 (mean 28.4 ± 496) (Timing of venipuncture on luteal phase, ie days 4-9 after ovulation). No participants were taking hormonal preparations.) Non-lesbian Salivary estradiol Mean age = 30 Technology, Executive Yuan and Taipei Veterans General Hospital. - Grant from the Central Research Fund Committee,
University of London. - Grant from Corroborated by score on SOM questionnaire . Self-reporting 25 2010 USA Downey 1987 USA n=5 Bisexual women n=7 Part of larger longitudinal study to study sexual identity development. Initial sampling at lesbian, gay, and bisexual community events, youth groups, and classes on gender and sexuality issues taught at local colleges and universities in interviews and online diary throughout longitudinal study. Homosexual women n=7 Recruitment by advertisement within a university community. Kinsey scale score based on partner preference of sexual fantasies and behavior and nonbisexual women who either identified as hetero-sexual or did not claim to have a sexual identity. These women had previously identified as lesbian or bisexual at the start of the longitudinal study. n=8 Recruiting the same as for lesbian and bisexual women. Hetero-sexual women n=7 Recruitment same as for homo-sexual women. years. (Timing of sample collection started 9
days after first day of menstrual period and consistent time of day. No participants were pregnant, breast feeding, or taking OCP at the time of sample collection.) Plasma Androstenedione Testosterone Age range: 19-29 (Timing of venipuncture on days 1-3 of menstrual cycle and between 8-9am on each day. Matching National Institutes of Child Health and Human Development. University of Utah Research Committee grant. - BRSG grant of the Research Foundation for Mental Hygiene; USPHS NIMH Research 26 during previous 12 months. Gartrell 1977 USA Homosexual women n=21 Recruitment: referred by local “homophile organizations”. Sexual behavior included only same-sex partners (homosexuals) or opposite sex partners (heterosexuals) for the preceding year. Heterosexual women n=19 No details of recruitment. Plasma Testosterone of homosexual and heterosexual participants according to: age, height, weight, level of education, and whether or not they had a live in partner. No
participants had irregular menstrual cycles, had used OCP in the previous year, or been exposed to diethylstilbestrol prenatally.) Age range homosexual women: 21-35; heterosexual women: 21-33. (Timing of venipuncture on days 1-3 of menstrual cycle and at 8am each day. No participants were taking OCP or had menstrual irregularities.) Scientist Development Award; Research Center Grants - No details 27 Gladue 1991 USA Gooren 1986 Netherland s Lesbians n=16 Recruited using newspaper ads, posters, referrals from friends and previous volunteers Categorized by Kinsey scale using information from questionnaires and interview data. Only included if exclusive lifelong (since puberty) homosexual or heterosexual history. Heterosexual women n=16 Recruitment same as lesbians women. Plasma Estradiol Testosterone (free and total) (Reference range not given but states results are in normal limits.) Age range: lesbians 21-32; heterosexual women: 27-21 (Timing of venipuncture on day 6 of
menstrual cycle and between 1-4pm on one day. No participants used OCP or had known endocrine abnormalities.) - Homosexual women n=6 No details of recruitment Self-reporting of orientation. Lesbians had a life-long history of exclusive or near Heterosexual women n=6 Plasma LH, Estradiol Testosterone Age range: homosexual women: 24-32; heterosexual women: 22-27. (Timing of venipuncture on day - No details of recruitment. Harry Frank Guggenheim Foundation; National Science Foundation Experimental Program to Stimulate Competitive Research; Achieving Science Excellence in North Dakota Project, National Science Foundation Research Experiences for Undergraduates Program. No details 28 exclusive homosexual orientation Griffiths 1974 Lesbian women: n=36 UK Juster 2016 Recruited through lesbian organizations Selfidentification as lesbian and member of lesbian organization “Normal” subjects from a previous study for estradiol, estriol and estrone n=not given Lesbian
women N=8 Bisexual women Selfidentification of orientation Heterosexual women n=20 3-5 of menstrual cycle between 8.3010am No participants had used hormonal preparations in 15 months before the study began.) Urinary Lesbians age 17-oxosteroids range: 22-55 (Comparator Epitestosterone population of an Estradiol, Estriol “appropriate age Estrone Prenanediol group” Timing of sampling in relation Pregnanetriol to menstrual cycle Testosterone (Reference ranges: was noted for lesbian subjects. pregnanediol: 6.2Comparator 15.6 (luteal) pregnanetriol: 0.3population samples taken at 8.9 “appropriate stage” 17-Oxosteroids: 17.4-559 of menstrual cycle. (µmol/24)5 Use of OCP was epitestosterone: 6.9- noted and taken 61.8 into account when reporting results.) testosterone: 3.5413 (nmol/24hr)) Salivary fasting Age range: 18-45 estradiol (Timing of sample Progesterone collection between - Endowment fund of St. Thomas Hospital Blood pressure BMI Canadian Institutes of Health 29
Canada n=13 Recruited as part of a broader research program. Separate advertisements according to sexual orientation. Loraine 1970 Lesbians n=4 No information on recruitment. by responding to one of three separate adverts asking for heterosexual, bisexual or lesbian participants and in telephone consultation. Corroborated using Klein Sexual Orientation Scale. Self-reporting of orientation and sexual behavior. Neave 1999 Lesbian women n=14 UK Recruited through homophile Self-reporting and score on questionnaire derived from UK Recruitment the same as for lesbian and bisexual women. Testosterone (Saliva) Plasma fasting DHEAS (DHEAS range: 1.2104 µmol/l) 12 noon and 7pm each day, phase of menstrual cycle not stated. Use of oral contraceptive use and phase of menstrual cycle was considered in analysis.) Cholesterol level Insulin level Triglyceride level Research. RP Juster Doctoral Scholarship from The Institute of Aging of Canadian Institutes of Health Research. Heterosexual
women n=not given Members of lab the staff who did not admit to homosexual inclinations. Heterosexual women n=14 Recruited from Urinary Epitestosterone FSH, LH Estradiol Estriol, Estrone Pregnanediol Testosterone Lesbians age range: 20-23 (age not given for controls). (Samples taken throughout menstrual cycle.) - No information Salivary Testosterone Age range: Lesbians: 19-43 (mean 26); Heterosexual - University of Northumbria Small Research 30 Singh 1999 USA organizations and friendship networks. sell scale of sexual orientation. Northumbria University student population and in the community matched to lesbian women in terms of education level and age. Lesbian women (n=33) separated into “butch” (n=17) and “femme” (n=16) categories according to score on personal history questionnaire. Recruited by “Snowball”/networkin g technique to find friends/acquaintance s of researchers who then recruited more participants by word Selfidentification as lesbian or
heterosexual Heterosexual women n=11 Same as for lesbian women Salivary Fasting: Testosterone women: 20-43 (mean 31), (Timing of sample collection according to menstrual cycle and consistent time of day. No participants were taking hormone influencing drugs (including OCP), had abnormal menstrual cycles, or had medical conditions affecting hormone level.) Age range: 25-45 (Timing of sample collection at 7-9am each day, phase of menstrual cycle not stated. No participants were taking OCP or had known ovarian problem.) Grants Scheme. BMI Age at menarche National Science Foundation Grant 31 Smith 2010 USA 455 456 of mouth. Lesbian women n=114 Recruitment using participants of the ESTHER Project who agreed to be contacted about further studies. Recruited to original study by local advertisement and community events Self-identified as nonheterosexual and reported only or primarily having emotional, physical, and romantic attraction towards women within the past 5 years or were
in relationships with only or primarily women within the past 5 years. Heterosexual women n=97 Self-identified as heterosexual/ straight and only had male partners since the age of 18. Plasma Fasting: Androstenedione Testosterone (Biochemical hyperandrogensism: tT ≥3.4ng/mL and A >2.4ng/mL) Age range: 35-45 (Venipuncture phase of menstrual cycle not stated. No participants were using OCP at time of venipuncture, displayed menopausal symptoms, or had a previous diagnosis of Cushing’s syndrome, androgen secreting tumors, congenital adrenal hyperplasia.) Acne BMI Hirsutism Infertility PCOS Oligomenorrhea ESTHER Project funded by National Lung, Blood and Heart Association. PCOS study funded by ESTHER Project, Lambda Foundation and Lesbian Health Fund (Gay and Lesbian Medical Association). Key: #Primary lesbians: Never had heterosexual experiences or interest, scored less than 20 on the heterosexual component of SOM. Intermediate 457 lesbians: Prior heterosexual experience or
interest and scored less than 20 on the heterosexual part of the SOM. Secondary Lesbians: Prior 459 Hormones: A: androstenedione; DHEAS: dehydroepiandrosterone sulphate; E2: estradiol; FAI: free androgen index (testosterone/ sex hormone 458 heterosexual experience or interest and scored more than 20 on the heterosexual part of the SOM (Dancey et al, 1990). 32 460 binding globulin x100); FSH: follicle stimulating hormone; L2: luteinizing hormone; P: progesterone; T: testosterone; fT: free testosterone, tT: total 462 Abbreviations: ESTHER – BMI – body mass index, BRSG – Biomedical Research support Grant, Epidemiologic Study of Health Risk. Nmol – 464 micromoles, USPHS NIMH – United States Public Health Service National Institute for Mental Health 461 testosterone. 463 nanomoles, OCP – oral contraceptive pill, PCO – polycystic ovaries, PCOS – polycystic ovary syndrome, SOM - sexual orientation method, µmol – 465 33 466 467 468 469 Table 2.
Hormone Levels, Showing Statistically Significantly Increased (↑), Decreased (↓), Same Levels (), or Not Measured () in Sexual Minority Women Compared to Heterosexual Women Without Known Ovarian Problems Author, date Androstene- DHEAS Epitestost- Estriol Estrone EstraFSH LH Pregnane- Progest- Testostdione erone diol diol erone erone Agrawal 2004 Dancey 1990p Dancey 1990i Dancey 1990s Diamond 2010 Downey 1987 Gartrell 1977 ↑ Gladue 1991 Gooren 1986 Griffiths 1974 ↓ ↑ Juster 2016 ↑ ↑ Loraine 1970 ↑ ↓ ↓ ↓ ↑ ↑ Neave 1999 Singh 1999 ↑ (“butch”) Singh 1999 (“femme”) Smith 2010 ACKNOWLEDGMENTS: We thank Miss Melanie Davies for comments on an earlier draft. We thank the anonymous peer reviewers and Editor on Chief for their comments. 34 REFERENCES 35 Agrawal, R., Sharma, S, Bekir, J,
Conway, G, Bailey, J, Balen, A H, & Prelevic, G (2004). Prevalence of polycystic ovaries and polycystic ovary syndrome in lesbian women compared with heterosexual women. Fertility & Sterility, 82(5), 1352-1357 doi:10.1016/jfertnstert200404041 Bailey, J. M, Vasey, P L, Diamond, L M, Breedlove, S M, Vilain, E, & Epprecht, M (2016). Sexual Orientation, Controversy, and Science Psychological Science in the Public Interest, 17(2), 45-101. doi:101177/1529100616637616 Balthazart, J. (2011) Minireview: Hormones and human sexual orientation Endocrinology, 152(8), 2937-2947. doi:101210/en2011-0277 Banks, A., & Gartrell, N K (1995) Hormones and sexual orientation: a questionable link Journal of Homosexuality, 28(3-4), 247-268. doi:101300/J082v28n03 04 Birke, L. I (1981) Is homosexuality hormonally determined? Journal of Homosexuality, 6(4), 35-49. Chen, C. H, Wang, P H, Hsieh, M T, Tzeng, C R, Wu, Y H, Lee, C S, Chu, H-Y, & Chang, H. Y (2014) Sexual orientations of women
with polycystic ovary syndrome: clinical observation in Taiwan. Taiwan Journal of Obstetrics and Gynecology, 53(4), 542-546 doi:10.1016/jtjog201409002 Cochran, S. D, & Mays, V M (2012) Risk of breast cancer mortality among women 36 cohabiting with same sex partners: findings from the National Health Interview Survey, 1997-2003. Journal of Womens Health, 21(5), 528-533 doi:101089/jwh20113134 Dancey, C. P (1990) Sexual orientation in women: an investigation of hormonal and personality variables. Biological Psychology, 30(3), 251-264 Diamond, L. M, & Wallen, K (2011) Sexual minority women's sexual motivation around the time of ovulation. Archives of Sexual Behavior, 40(2), 237-246 doi:101007/s10508-0109631-2 Downey, J., Ehrhardt, A A, Schiffman, M, Dyrenfurth, I, & Becker, J (1987) Sex hormones in lesbian and heterosexual women. Hormones and Behavior, 21(3), 347-357 Gartrell, N. K, Loriaux, D L, & Chase, T N (1977) Plasma testosterone in homosexual and
heterosexual women. American Journal of Psychiatry, 134(10), 1117-1118 doi:10.1176/ajp134101117 Gladue, B. A (1991) Aggressive Behavioral Characteristics, Hormones and Sexual Orientation in Men and Women. Aggressive Behavior, 17, 313-326 Gooren, L. (1986) The neuroendocrine response of luteinizing hormone to estrogen administration in heterosexual, homosexual, and transsexual subjects. Journal of Clinical Endocrinology and Metabolism, 63(3), 583-588. doi:101210/jcem-63-3-583 Griffiths, P. D, Merry, J, Browning, M C, Eisinger, A J, Huntsman, R G, Lord, E J, 37 Whitehouse, R. H (1974) Homosexual women: an endocrine and psychological study Journal of Endocrinology, 63(3), 549-556 James, W. H (2005) Biological and psychosocial determinants of male and female human sexual orientation. Journal of Biosocial Science, 37(5), 555-567 doi:10.1017/S0021932004007059 Juster, R. P, Almeida, D, Cardoso, C, Raymond, C, Johnson, P J, Pfaus, J G, Lupien, S. J (2016) Gonads and strife: Sex
hormones vary according to sexual orientation for women and stress indices for both sexes. Psychoneuroendocrinology, 72, 119-130 doi:10.1016/jpsyneuen201606011 Lalumière M.L, Blanchard R, & Zucker KJ (2000) Sexual orientation and handedness in men and women: a meta-analysis. Psychological Bulletin, 126(4), 575-92 Loraine, J. A, Ismail, A A, Adamopoulos, D A, & Dove, G A (1970) Endocrine function in male and female homosexuals. British Medical Journal, 4(5732), 406-409 Meads, C., Martin, A, Grierson, J, & Varney, J (2018) Systematic review and metaanalysis of diabetes mellitus, cardiovascular and respiratory condition epidemiology in sexual minority women. BMJ Open, 8(4), e020776 doi:101136/bmjopen-2017-020776 Meads, C., & Moore, D (2013) Breast cancer in lesbians and bisexual women: systematic 38 review of incidence, prevalence and risk studies. BMC Public Health, 13, 1127 doi:10.1186/1471-2458-13-1127 Meyer-Bahlburg, H. F (1979) Sex hormones and female
homosexuality: a critical examination. Archives of Sexual Behavior, 8(2), 101-119 Meyer, I. H (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129(5), 674697 doi:101037/0033-29091295674 Neave, N., Menaged, M, & Weightman, D R (1999) Sex differences in cognition: the role of testosterone and sexual orientation. Brain and Cognition, 41(3), 245-262 doi:10.1006/brcg19991125 O'Hanlan, K. A, Gordon, J C, & Sullivan, M W (2018) Biological origins of sexual orientation and gender identity: Impact on health. Gynecologic Oncology, 149(1), 33-42 doi:10.1016/jygyno201711014 Pearcey, S. M, Docherty, K J, & Dabbs, J M, Jr (1996) Testosterone and sex role identification in lesbian couples. Physiology & Behavior, 60(3), 1033-1035 Robinson, K., Galloway, K Y, Bewley, S, & Meads, C (2017) Lesbian and bisexual women's gynaecological conditions: a systematic
review and exploratory meta-analysis. BJOG, 124(3), 381-392. doi:101111/1471-052814414 39 Singh, D., Vidaurri, M, Zambarano, R J, & Dabbs, J M, Jr (1999) Lesbian erotic role identification: behavioral, morphological, and hormonal correlates. Journal of Personality and Social Psychology, 76(6), 1035-1049. Smith, H. A, Markovic, N, Matthews, A K, Danielson, M E, Kalro, B N, Youk, A O, & Talbott, E. O (2011) A comparison of polycystic ovary syndrome and related factors between lesbian and heterosexual women. Womens Health Issues, 21(3), 191-198 doi:10.1016/jwhi201011001 Stout, S. A, Litvak, M, Robbins, N M, & Sandberg, D E (2010) Congenital adrenal hyperplasia: classification of studies employing psychological endpoints. International Journal of Pediatric Endocrinology, 2010, 191520. doi:101155/2010/191520 Swift-Gallant, A., Johnson, B A, Di Rita, V, & Breedlove, S B (2020) Through a glass, darkly: Human digit ratios reflect prenatal androgens, imperfectly. Hormones
and Behavior, 120, 104686. doiorg/101016/jyhbeh2020104686 Van Wyk, P. H, & Geist, C S (1995) Biology of bisexuality: critique and observations Journal of Homosexuality, 28(3-4), 357-373. doi:101300/J082v28n03 11 40 Online supplement material Sex Hormone Levels in Lesbian, Bisexual, and Heterosexual Women: Systematic Review & Exploratory Meta-analysis Online Supplement Contents: Search Terms Used and Search Strategy for At Least One Database Data Extraction Form Table 1 - Full Text Excluded Studies with Reasons for Exclusion Table 2 - Quality Assessment of Included Studies Table 3 – Plasma Hormone Results Table 4 - Saliva Hormone Results Table 5 - Urine Hormone Results Figure 1 – PRISMA Flow Diagram 41 Search Terms Used and Search Strategy for At Least One Database Search Terms Used on First and Second Round of Literature Searching (Lesbian OR Bisexual OR Homosexual) AND Hormone OR ?estrogen OR Androgen OR Testosterone OR Progesterone OR LH OR FSH OR GnRH OR
ACTH OR CRH OR Activin OR Inhibin Literature Searching Customized to Each Database. Database Customization of Search Search Type Used Pubmed Term “Homosexual” not included Title and Abstract as clearly covered in MeSH terms CENTRAL - Titles, Abstracts, Key Words EMBASE - Abstract British Nursing “?” omitted from ?estrogen as Index search engine did not Abstract understand function Web of Science - Topic Psych Info - Abstract Data Extraction Form Name of Study Authors Year of Publication Study Type Setting Method of Recruitment Funding Country Timescale Aim of Study Exposure Outcome Size of Study Populations Age Range Inclusion Criteria Exclusion Criteria Comparator Population Hormones Measured Method Timing of Hormone Measurement Hormone Related Conditions Measured Additional Tests/Investigations Determination of Sexual Orientation Additional Diagnostic Criteria Hormone 42 Study Demographics Population Description Comments Lesbian Bisexual
Heterosexual Methods Description Comments Fasting Menstrual Diurnal Unit Hormonal Data Lesbian Bisexual 43 Hormone Reference Ranges Condition/Variable Measured Statistical Analysis Notes Additional Data Unit Lesbian Bisexual Online Supplement Table 1: Excluded Studies with Reasons for Exclusion Author, Year Baker et al. 2002 Juster et al. 2015 Title Testosterone, Alcohol and Civil and Rough Conflict Resolution Strategies in Lesbian Couples Oral Contraceptives, Androgens and the Sexuality of Young Women: II. The Role of Androgens Is Homosexuality Hormonally Determined? PCOS in Lesbian and Heterosexual Women Treated with Artificial Donor Insemination. Testing the Affiliation Hypothesis of Homoerotic Motivation in Humans: The Effects of Progesterone and Priming Neuroendocrine Response to Estrogen and Sexual Orientation Significance of Androgen Levels in the Aetiology and Treatment of Homosexuality Sexual Orientation Modulates Endocrine Stress Reactivity Loraine et al.
1971 Patterns of Hormone Excretion in Male and Female Homosexuals Pearcey et al. 1995 Testosterone and Sex Role Identification in Lesbian Couples Bancroft et al. 1991 Birke 2012 De Sutter et al. 2008 Fleischman et al. 2014 Gladue et al. 1984 James et al. 1977 44 Reason for Exclusion No heterosexual control group or normal reference range to use as control Hormonal data only for women using OCP or not. No data grouped by sexual orientation Review article Hormone levels not included in final analysis as too many patients data was missing Progesterone levels not separated according to sexual orientation No data on lesbian or bisexual women Study on males only No data on sex hormone levels only how sex hormones affect cortisol Further discussion of an earlier study already being used in this SR No heterosexual control group or normal reference range to use as control Online Supplement Table 2: Plasma Hormone Results Study Method Hormone Year Timing (Units) Agrawal et
Venipuncture on day 2 or 3 of al. Chen et al. 2014 Populations and results given as mean and (SD) Lesbians menstrual cycle. 2004 45 P value Statistical Significance Test L vs. H1 Two tailed t Heterosexuals NO PCO PCOS NO PCO PCOS PCO PCOS (n=51) (n=107) (n=97) (n=248) (n=65) (n=51) A (nmol/L) - 7.032 12.82 - 6.092 8.132 NS <0.001* DHEAS (µg/ml) 3.7 (08) 6.1 (1) 7.4 (16) 4.9 (09) 4.9 (08) 6 (1.2) NS NS E2 (pmol/l) 162 (32) 169 (36) 170 (45) 162 (35) 156 (28) 169 (43) NS NS FAI - 3.752 12.032 - 2.52 5.632 <0.01* <0.001* FSH (IU/l) 7.7 (14) 6.9 (12) 5.4 (09) 7.9 (16) 6.5 (13) 6 (0.7) NS NS LH (IU/l) 4.5 (05) 4.8 (04) 7.8 (09) 4.4 (05) 4.8 (03) 7.3 (10) NS NS Prolactin (mIU/L) 412 (56) 364 (40) 376 (40) 340 (43) 365 (34) 362 (34) NS NS T (nmol/L) - 2.032 3.442 - 1.722 2.662 <0.05* <0.05* tests, MannWhitney U tests (details not given as to which tests used for each hormone)
Lesbians with PCOS (n=8) Heterosexuals with PCOS (n=89) L vs. H Unpaired t A (ng/ml) 2.4 (10) 2.4 (15) 0.936 test E2 (pmol/l) 59.1 (134) 129.7 (1512) <0.001* FAI 0.08 (004) 0.07 (011) 0.790 FSH (IU/l) 5.7 (13) 5.6 (21) 0.874 Fasting venipuncture Dancey LH/FSH ratio 2.20 (065) 2.90 (180) 0.242 LH (IU/l) 12.7 (51) 15.1 (81) 0.422 Prolactin (ng/mL) 21.2 (133) 13.3 (63) 0.141 T (ng/ml) 0.34 (013) 0.41 (024) 0.432 PL (n=10) Venipuncture during luteal IL (n=10) SL (n=10) H (n=10) ovulation) of menstrual cycle. A (nmol/L) 8.29 (359) 7.69 (237) 9.38 (372) 9.52 (418) 0.69 Ovulation kits used to E2 (pmol/L) 408.44 (27503) 306.8 (1282) 463.7 (20004) 424.5 (17516) 0.31 determine point in cycle. P (nmol/L) 23.7 (1511) 28.5 (2337) 25.2 (1956) 29.9 (2908) 0.98 T (nmol/L) 2.24 (058) 1.98 (088) 2.58 (135) 2.56 (130) 0.58 T/P (ratio) 0.17 (017) 0.17 (021) 0.53 (075) 0.34 (047) 0.90 Downey et Venipuncture between 8 and
al. 9am on 1st, 2nd and 3rd days of menstrual period1. Average of 1987 Gartrell et al. Lesbians (n=7) Heterosexuals (n=7) L vs. H A (ng/100ml) 112 (19) 124 (36) NS T (ng/100ml) 32 (12) 32 (5) NS Lesbians (n=21) Heterosexuals(n=19) L vs. H Details not 36 (11) 26 (7) <0.001* given t tests 3 specimens. Venipuncture at 8am of days 1, 2 and 3 of menstrual 1977 ANOVA all 4 groups phase (day 4-9 after 1990 ANOVA run across 46 cycle3. Average of three samples taken. T (ng/100mL) Gladue 1991 Gooren et al. Venipuncture on day 6 of No details Not given No details LB vs. H ANCOVA 41.4 (149) 36.9 (92) and 4pm. Two samples taken fT (pg/ml) 1.75 (07) 2.31 (12) one hour apart. tT (ng/dl) 47 (18) 37 (10) Lesbians (n=6) Heterosexuals (n=6) E2 (pg/ml) 36 (9) 34 (10) LH (mIU/ml) 5.2 (12) 5.0 (10) T (ng/ml) 0.29 (011) 0.32 (01) Fasting venipuncture between LB Heterosexual 8am and 11am (n=20) (n=20) 7.34 (064) 5.58 (037) 0.027*
Lesbians (n=114) Heterosexuals (n=97) L vs. H Wilcoxon Venipuncture during days 3-6 2016 2010 Not given E2 (pg/ml) 1986 Smith et al. Heterosexuals (n=16) menstrual cycle between 1 of menstrual cycle Juster et al. Lesbians (n=16) 47 DHEAS µmol/l Analysis carried out on blood stored from previous study A (ng/ml) 1.63 (median) 1.51 (median) 0.079 rank-sum (fasting venipuncture). T (ng/ml) 1.69 (median) 1.52 (median) 0.069 tests Key: Hormones: A: androstenedione; DHEAS: dehydroepiandrosterone sulphate; E2: estradiol; FAI: free androgen index (testosterone/SHBGx100); FSH: follicle stimulating hormone; L2: luteinising hormone; P: progesterone; T: testosterone; fT: free testosterone, tT: total testosterone. Populations: H: heterosexual women; IL: intermediate lesbians; L: lesbians; LB: lesbian and bisexual women; PL: primary lesbians; SL: secondary lesbians. Dancey et al (1990 defines these as Primary – lesbians with no heterosexual interest or experience, and
scored less than 20 on the Sexual Orientation Method questionnaire, Intermediate - lesbians with prior heterosexual interest or experience, and scored less than 20 on the Sexual Orientation Method 48 questionnaire, Secondary - lesbians with prior heterosexual interest or experience and scored more than 20 on the Sexual Orientation Method questionnaire. Conditions: NO: normal ovaries; PCO: polycystic ovaries; PCOS: polycystic ovary syndrome. Statistics: ANOVA: analysis of variance; ANCOVA: analysis of covariance. NS: not significant 1 Statistical significance was analysed in all hormones for which levels are given All differences in women with normal ovaries were not significant. 2Data extracted from graphs; (med): value is median NOT mean 3Day 1 defined as 8am which occurred within 24 hours of menstrual onset. *Statistically significant result: 49 Online Supplement Table 3: Saliva Hormone Results Study Method Hormone Year Timing (unit) Diamond Daily saliva samples for
10 days at 2010 the same time each day starting on E2 (pg/ml) Population and results given as mean and (SD) L (n=5) B (n=7) NLB (n=8) 1.9 (05) 1.9 (07) 2.2 (19) P value Statistical Significance test Not given No details ANCOVA day 9 of menstrual cycle. Juster 2016 LB (n=20) H (n=20) LB vs. H E2 (pg/ml) 4.33 (042)1 4.58 (458)1 NS P (pg/ml) 122.92 (1667)1 66.67 (1667)1 <0.05* T (pg/ml) 64.44 (444)1 48.89 (444)1 0.006* Saliva samples produced at same Lesbians Heterosexuals Homosexual men/women vs. stage in menstrual cycle at 10am- (n=13) (n=12) heterosexual men + women 37.50 (833) 1 22.22 (556)1 0.06 Saliva sample taken between 12pm and 7pm. Neave 1999 12pm or 2pm-4pm over 2 months. Singh 1999 T (pg/ml) Fasting saliva sample between 7 Butch L Femme L H and 9am (n=17) (n=16) (n=11) 4.1 (17) 2.5 (08) 2.3 (09) T (ng/ml) BuL vs. FL BuL vs. H FL vs. H <0.001* <0.001* 0.99 ANOVA ANOVA Hormones: E2: estradiol; P:
progesterone; T: testosterone. Populations: B: bisexuals; BuL: butch lesbians; FL: femme lesbians; H: heterosexual women; L: lesbian; LB: lesbians and bisexuals; NLB: no longer lesbian or bisexual identity. Statistics: ANOVA: analysis of variance; ANCOVA: analysis of covariance; NS: not significant 1Data extracted from graphs. *Statistically significant result. 50 Online Supplement Table 4 - Urine Hormone Results Study Method Hormone Year Timing (Units) Griffiths Urine et al. sample timing in 1974 Population and results given as mean and (SD) P value Significance Lesbians (n=36) Reference Range 17-O (μmol/24hr) 28.8 (69-743) 17.4-5591 E1 (nmol/24hr) 8.1 (0-483) Onset of menses:14.8-258; Ovulation peak: 406-1144; Luteal: relation to Not given No details 36.9-8492 menstrual E2 (nmol/24hr) 4.4 (0-165) Onset of menses: 0-11; Ovulation peak: 14.7-514; Luteal: 147-3672 cycle was E3 (nmol/24hr) 26.6 (0-1183) Onset of menses: 0-51.9; Ovulation peak:
45-1868; 277-29412 noted. Pgn2 (μmol/24hr) 9.7 (28-300) Follicular: <3.12; Luteal: 62-1561 Pgn3 (μmol/24hr) 1.8 (006-39) 0.3-891 T (nmol/24hr) 33.7 (0-913) 3.5-4133 eT (nmol/24hr) 33.0 (0-1024) 6.9-6183 Loraine 48 hour L1 L2 L3 L4 L Mean4 H et al. pools of (n=1) (n=1) (n=1) (n=1) (n=4) (n=not L vs. H No details given) urine 1970 Test produced E1 (μmol/24hr) 6.7 (29) 7.1 (45) 1.5 (29) 1.1 (22) 4.1 (31) 9.5 (48) All comparisons <0.05-0001* throughou E2 (μmol/24hr) 3.9 (17) 3.7 (32) 1.1 (24) 0.5 (05) 2.3 (20) 3.5 (24) L1,L2 p=NS, L3,L4 p<0.001* . t cycle. E3 (μmol/24hr) 11.0 (6) 6.5 (44) 13.6 (97) 3.8 (22) 8.7 (56) 9.7 (65) Results L1,L3 p=NS, L2 p<0.01, L4 p<0.001 given as FSH (IU/24hr) 9.0 (73) 10.4 (131) 3.6 (20) 6.0 (49) 7.3 (68) 7.3 (18) L1,L2,L4 p=NS L3 p<0.001 value per LH (IU/24hr) 12.4 (223) 26.0 (232) 37.1 (312) 30.7 (295) 26.6 (265) 11.1 (41) L1 p=NS, L2, L4 p <0.05,
24 hours. L3 p<0.01 Pgn2 (mg/24hr) 1.4 (07) 2.0 (15) 0.5 (05) 1.0 (10) 1.2 (09) 1.2 (17) L1,L3,L4 p=NS, L2 p<0.001 T (μmol/24hr) 11 (1.8) 17.3 (26) 16.0 (25) 30.0 (53) 18.6 (31) 7.3 (43) All comparisons <0.05-0001* eT (μmol/24hr) 9.2 (65) 18.2 (75) 14.1 (105) 14.1 (102) 13.9 (87) 8.9 (48) L1,L3,L4 p=NS, L2 p<0.001 Key: 17-O: 17-oxosteroids; E1: estrone; E2: estradiol; E3: estriol; FSH: follicle stimulating hormone; L2: luteinising hormone; Pgn2: pregnanediol; Pgn3: pregnanetriol; T: testosterone; eT: epitestosterone. S: Significant 1Textbook values from “Hormone Assays and their Clinical Applications (Loraine and Bell 1966).2: “Normal” appears to heavily imply heterosexual (or at least not lesbian) but this is not explicit (Brown 1955) 3Textbook values taken from “Gas Chromatographic Determination of Normal Steroids” (Inguilla et al, 1976). 4Individual means given for each lesbian participant (n=4), mean calculated in Microsoft Excel
during this systematic review for comparative purposes, values given to one decimal place as in study. *Statistically significant result. 51 52 Online Supplement Table 5 - Quality Assessment of Included Studies Study Study Selection Biases Performance Design Biases Agrawal 2004 Cohort Study Consecutive private clinic sample where SMW attending for different reasons to heterosexual women (single and partnered) and partners of SMW. Possibility of misclassification of single women As participants from the different groups attending for different reasons, clinical treatment of each group was different. Attrition Biases Detection Biases Chen 2014 Cross sectional analysis Clinic sample. Unclear if consecutive or not. All have PCOS Not reported Hormone assays similar in all groups. Blinding unclear. Dancey 1990 Case-Control Volunteer sample from community. Paid £12 plus travel expenses – this may have biased volunteering. Unclear if SMW and heterosexual women attending
clinic for the same reason None reported Hormone assays similar in all groups. Blinding unclear. Diamond 2010 Cohort Study Subsample of a larger cohort study investigating sexual identity development. Paid $60 – this may have biased volunteering. None reported The first 10 blood assays from each group were used, possibly introducing bias as later ones discarded There had been 33 participants but 13 gave incomplete data. Downey 1987 Case-Control Volunteer sample from university community. None reported Not reported Gartrell 1977 Case-Control None reported Not reported Gladue 1991 Cross-sectional Study None reported Not reported Gooren 1986 Case-Control Referred sample from ‘homophile organisations’. Unclear where heterosexual sample from. Undergraduate sample volunteering in return for research credits. Possibility of misclassification of sexual orientation. Recruitment method not reported. Hormone assays similar in both groups. Assays done blind to group.
Hormone assays similar in both groups. Blinding unclear. Hormone assays similar in both groups. Blinding unclear. None reported Not reported Not reported Hormone assays similar in all groups. Blinding unclear. Results not given separately for the separate groups. Hormone assays similar in all groups. Blinding unclear. Hormone assays Comment Pathologising of SMW by suggesting 80% have a problem (PCO) whereas the medical condition is PCOS – 38% SMW. No ethics permission statement Excluded second control group without PCOS as no indication of sexual orientation. Unusual separation into ‘primary’, ‘intermediate’ and ‘secondary’ lesbians. Bisexual group excluded as too few. Heteronormative classification of ‘gave up lesbian/bisexual identity’ No ethics permission statement No ethics permission statement No ethics permission statement No ethics permission statement - Study Study Design Selection Biases Performance Biases Attrition Biases Griffiths 1974
Cross-Sectional analysis Lesbians from membership of a lesbian organisation. Comparator was a group of ‘like-aged mothers of a sample of normal children’. Subsample from a larger study, recruitment method not reported. Paid $50 CAD – this may have biased volunteering. Lesbian recruitment method not reported. Controls were members of scientific and technical staff. Possibility of misclassification of sexual orientation. Lesbian volunteers from ‘homophile organisations and friendship networks’ Controls were university students and non-university participants. Recruitment through snowballing or networking via friends and acquaintances of the researchers. Comparator group not sampled at the same time as the lesbian group None reported There were 42 lesbian volunteers but only 36 provided hormone samples Not reported Juster 2016 Cross-sectional analysis Loraine 1970 Case-control study None reported Neave 1999 Case-Control study Singh 1999 Cross-Sectional Analysis
Smith 2010 Cross-Sectional Analysis Subsample from a larger study. Community volunteer sample. Study investigating PCOS, diagnosed blind to sexual orientation. Detection Biases Comment 53 similar in both groups. Blinding unclear. Basal hormone assay levels used only Normal values used for comparator. No ethics permission statement Hormone assay similar in both groups. Blinding unclear. Absolute values for testosterone, estradiol and progesterone not reported. Not reported Lesbian assay results not averaged. No ethics permission statement None reported Testosterone not measured in 2 controls. - None reported Not reported Hormone assay similar in both groups. Blinding unclear. Testosterone levels estimated from graphs. Hormone assay similar in both groups. Blinding unclear. None reported Not reported Hormone assay similar in both groups. Blinding unclear. SMW ‘butch’ and ‘femme’ categories. Study 2 used only. No ethics permission statement Since more women
in the lesbian group had PCOS (7.9%) than in the heterosexual group (4.1%) the mean testosterone levels will be higher in the lesbian group. 54 1 9 10 11 17 18 23 24 Online Supplement Figure 1 – PRISMA Flow Diagram 2 3 Citations Citations 4 identified from identified from reference lists 5 database 6 N=9 searches 7 N=1227 8 Abstracts read in full N=104 12 13 14 15 16 Full texts read in full N=24 19 20 21 22 Included in systematic review N=14 Included in meta-analysis N=9 Citations excluded from title as irrelevant N=1123 Citations excluded from abstract N=71 Studies excluded N=10 (see Table)