Datasheet
Year, pagecount:2013, 22 page(s)
Language:English
Downloads:2
Uploaded:June 15, 2023
Size:4 MB
Institution:
-
Comments:
Attachment:-
Download in PDF:Please log in!
Comments
No comments yet. You can be the first!
Most popular documents in this category
Content extract
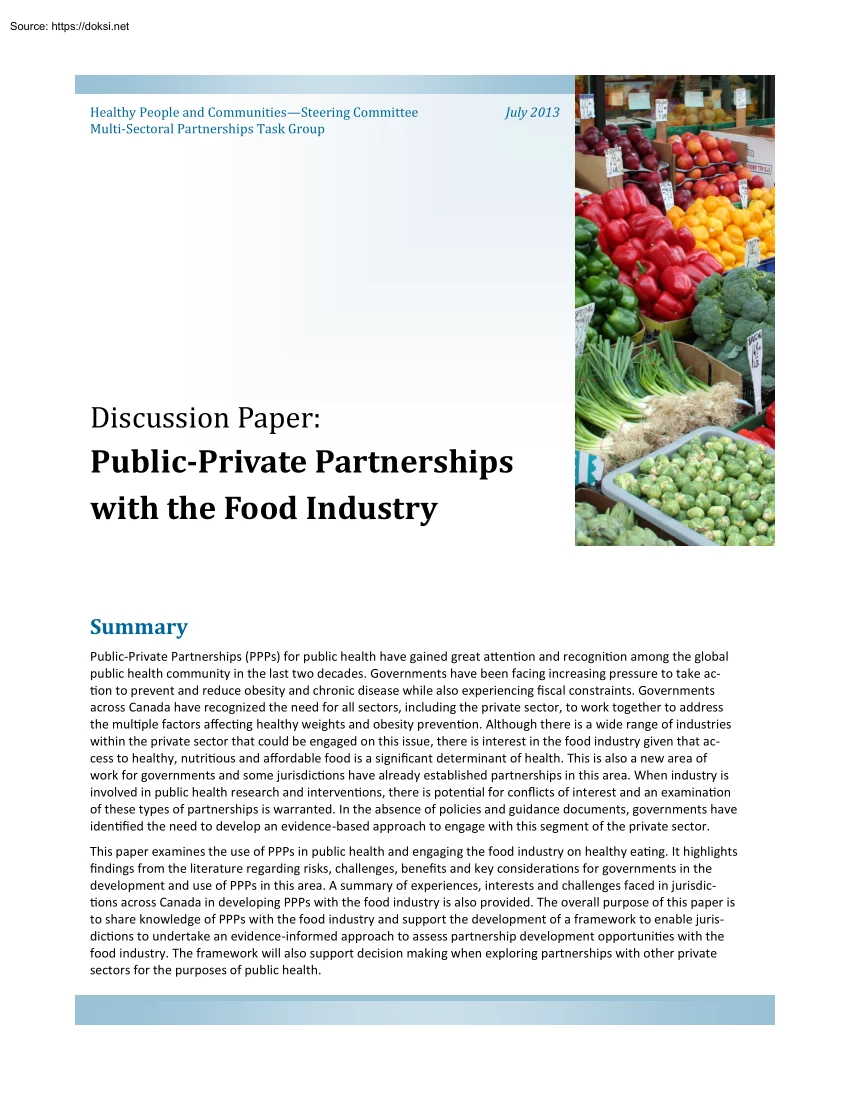
Healthy People and CommunitiesSteering Committee Multi-Sectoral Partnerships Task Group July 2013 Discussion Paper: Public-Private Partnerships with the Food Industry Summary Public-Private Partnerships (PPPs) for public health have gained great attention and recognition among the global public health community in the last two decades. Governments have been facing increasing pressure to take action to prevent and reduce obesity and chronic disease while also experiencing fiscal constraints Governments across Canada have recognized the need for all sectors, including the private sector, to work together to address the multiple factors affecting healthy weights and obesity prevention. Although there is a wide range of industries within the private sector that could be engaged on this issue, there is interest in the food industry given that access to healthy, nutritious and affordable food is a significant determinant of health. This is also a new area of work for governments and some
jurisdictions have already established partnerships in this area. When industry is involved in public health research and interventions, there is potential for conflicts of interest and an examination of these types of partnerships is warranted. In the absence of policies and guidance documents, governments have identified the need to develop an evidence-based approach to engage with this segment of the private sector. This paper examines the use of PPPs in public health and engaging the food industry on healthy eating. It highlights findings from the literature regarding risks, challenges, benefits and key considerations for governments in the development and use of PPPs in this area. A summary of experiences, interests and challenges faced in jurisdictions across Canada in developing PPPs with the food industry is also provided The overall purpose of this paper is to share knowledge of PPPs with the food industry and support the development of a framework to enable jurisdictions to
undertake an evidence-informed approach to assess partnership development opportunities with the food industry. The framework will also support decision making when exploring partnerships with other private sectors for the purposes of public health. Purpose and Scope In September 2010, Federal-Provincial/Territorial (F-P/T) Ministers of Health and/or Healthy Living/Health Promotion endorsed a Declaration on Prevention and Promotion and committed to making the promotion of health and the prevention of disease, disability and injury a shared priority for action. As the first commitment of the Declaration, Ministers endorsed the Curbing Childhood Obesity: A Federal, Provincial and Territorial Framework for Action to Promote Healthy Weights (Healthy Weights Framework) and committed to working together and with other sectors on joint actions that will help Canadians live longer, healthier lives. In November 2011, all Ministers (except Quebec) released a report entitled Actions Taken and
Future Directions 2011 (Healthy Weights Report). The report proposes recommendations and actions that can be taken by Ministers of Health and their respective governments, as well as other sectors, to advance efforts to curb childhood obesity. “Over the last two decades, PPPs for public health have gained great attention and recognition among the global public health community” Key Terms Public-private partnerships in public health are defined as at least one representatives from government and one from the private-for-profit sector working together to achieve a shared public health objective based on some degree of shared decision-making. The food industry is made up of growers, producers, manufacturers, distributors, retailers and their associations that range in size from smallmedium enterprises to large multi-national corporations. Partnerships on healthy eating cover a range of activities related to healthy weights, obesity prevention, diet and nutrition. 2 The Healthy
Weights Report recognizes the need for all sectors, including the private sector, to work together to address the multiple factors affecting childhood obesity across Canada. There are a number of strategies within the Healthy Weights Framework that governments can collaborate with the private sector on, including: Increasing the availability and accessibility of nutritious food; Decreasing marketing of food and beverages high in fat, sugar and/or sodium to children; and, Improving the physical environment where children live, learn and play to promote physical activity. Over the last two decades, public-private partnerships (PPPs) for public health have gained great attention and recognition among the global public health community as a strategy to potentially overcome barriers that otherwise neither sector could respond to on its own (Widdus, 2005; Reich, Hershey, Hardy, Childress & Bernheim, 2003). Governments have been facing increasing pressure to take action to
prevent and reduce obesity and chronic disease while experiencing fiscal constraints. This has made PPPs an attractive mechanism to collaborate with the private sector to address obesity and chronic disease prevention (De Pinho, 2012). For the purposes of this paper, public-private partnerships in public health are defined as at least one representative from government and one from the private-for-profit sector working together to achieve a shared public health objective based on some degree of shared decision-making. There are a wide range of industries within the private sector that could be engaged to address issues related to healthy eating, including: the food industry (producers, manufacturers, distributors, retailers and associations), health care (insurance and pharmaceuticals), sports and athletics industry Research Methodology (teams, equipment and apparel) and children’s products and entertainments (toys, games, TV and other media). This paper focuses on the food
industry given that access to healthy, nutritious and affordable food is a significant determinant of health. The food industry is made up of growers, producers, manufacturers, distributors, retailers and their associations that range in size from small-medium enterprises to large multi-national corporations. For the purposes of this paper, partnerships on healthy eating cover a range of activities related to healthy weights, obesity prevention, diet and nutrition. This paper will highlight findings from the literature regarding benefits and challenges of engaging with certain segments of the food industry on healthy eating. This discussion paper is based on the findings of two independent literature reviews conducted by Ontario and Health Canada. The review completed by Ontario, examined the literature on PPPs for public health with an emphasis on diet, nutrition and obesity prevention. It examined reasons for engaging in PPPs in public health, contentious issues, engagement models
and barriers to working with industry on obesity prevention. The review completed by Health Canada focused on research regarding benefits and risks of collaborating with the private sector on public health issues. It examined the food industry and several important factors for government to consider before developing these arrangements, such as conflict of interest. Collaborating with the food industry to support healthy eating is a new area of work for government. Policies have been established to address PPPs with other sectors, such as tobacco, alcohol and pharmaceuticals; however, there are no guiding documents in place when it comes to the food industry. Governments have identified the need to develop an evidence-based approach to support their decision-making process in this area. This paper aims to share knowledge of PPPs with the food industry and support a national dialogue on this issue. It is the first step in developing a national framework that will support jurisdictions
to undertake an evidence-informed approach when assessing whether and with whom to partner with to support healthy eating initiatives. It highlights findings from the literature regarding risks, challenges, benefits and key considerations for governments in the development and use of PPPs in this area. Although it is out of scope for this paper, it is recognized that other areas of government (outside of public health) are engaged with the food industry and health/healthy living ministries may want to recommend that a ‘health in all public policy’ approach be adopted. This would limit all government activities with companies in the food industry whose activities conflict with public health goals in the same way governments have restricted activities with tobacco companies. 3 Public-Private Partnerships in Public Health The literature on PPPs for public health lacks a well-grounded conceptualization of the term “public-private partnership”. The term “partnership” is
used loosely with no consensus around its definition (Field & Peck, 2003), is loaded with ambiguities (Asante & Zwi, 2007) and has become a buzzword in the field (Van Huijstee, Francken & Leroy 2007). It is often difficult to distinguish the meaning of partnerships from other forms of cross-organizational activities such as building an alliance, collaborating, cooperating, networking and joint-working (Huxham, Vangen Huxham & Eden, 2000). Within the field of public health, PPPs are described as any form of engagement or interaction between the public and the private sectors (Hawkes, 2008) However, different forms of engagement have varying degrees of complexity and can be placed along a continuum (Table 1). In which case, partnerships appear at the end of the continuum due to their higher complexity and structured, formal arrangements (Rowitz, 2006). Table 1: Forms of Engagement with the Private Sector Donation Charitable financial or in-kind donations that enhance each
partner’s brand image. Platforms for Discussion Sponsorship Alliances Partnerships Platforms for discussion are often created for information sharing. They bring together different actors to map out strategies for addressing changes. Any form of monetary or inkind payment or contribution to an event, activity or individual that promotes a company’s name, brand, products or services. Alliances are groups of organizations that combine forces to address specific public health issues. They create informal agreements to provide programs or services to the community. A partnership is a mechanism based on shared decision-making that brings together a diversity of skills and resources of various organizations in innovative ways to improve specific outcomes. Lower-level of Complexity Higher-level of Complexity There are important elements that distinguish these forms of engagement which influence how it is designed, implemented and evaluated. For example, a “platform for
discussion” is often created to share information and has no formal governance structure. On the other hand, “partnerships” are more formal and encompass a set of key elements, such as: the presence of multiple actors; having shared goals; developing commitments, roles and responsibilities as part of the agreement; a mutually agreed division of resources and expertise; and, a decision-making process negotiated among partner organizations (Ridley, 2001; Buse & Waxman, 2001; Widdus, 2005; Reich, 2000; Peters, 1998; The Canadian Council for Public-Private Partnerships, 2011). 4 Another difficulty with the term PPPs is determining what constitutes the “public” and the “private” sectors (Reich, 2000; Hawkes, 2008; Buse & Walt, 2000; Kickbusch & Lister, 2006). In this paper, the “public sector” refers to any level of government or governmental agency and the “private sector” refers to for-profit organizations, associations representing for-profit
organizations or private foundations (e.g the Bill and Melinda Gates Foundation) Non-profit organizations and inter-governmental agencies, such as the World Health Organization, are considered the third party within PPPs. These differences can be fundamental as they have implications for governance, accountability, values and ethical considerations (De Pinho, 2012) Types of Partnerships in Public Health Public-private partnerships within the public health sector are not a new development and have been taking place since the early 2000s. Within the literature, the predominant form of classification is based on the goals or objectives of the partnership (Reich, 2002) Using a goal oriented classification, the majority of PPPs have been found to cluster into partnerships for disease control, which in turn is split into two categories of partnerships. Firstly, PPPs for product development, which focuses on research and development of drugs, vaccines and new diagnostics, and secondly, PPPs
for access to drug and vaccines, involving the provision of discounted or donated drugs and vaccines (Widdus, 2005). Additionally, PPPs for strengthening health services, (Dewan , Lal, Lonnroth, Wares, Uplekar, Sahu, et al, 2006; Newell, Pande , Baral, Bam, & Malla 2005; Balasubramanian, Rajeswari & Vijayabhaskara et al, 2006; Boyle, Gardner & Callaway 1998; Lonnroth, Uplekar & Arora et al, 2004), improving advocacy and education (Clasen, 2002; Bravo, 2007; Yerby, 1998; Meredith & Ziemba, 2007), improving regulation, quality and standards (The Pharmaceutical Security Institute, 2011) and global financing coordination (Hardon, 2001; Levine, Cherian , Shah & Batson, 2004) are among the subset of goal-oriented PPPs. The organizational structures of PPPs are inherently different as partnerships are considered context specific (De Pinho, 2012). PPPs can be structured in a way that they are legally dependent, not-for-profit organizations, such as Medicine for Malaria
Ventures (MMV) and Global Alliance for Vaccines and Immunization (GAVI) (De Pinho Campos, Norman & Jadad, 2011). Others are less structured and have been designed as informal collaboration between the public and private for-profit health providers in the form of socialmarketing activities, vouchers, pre-packaging, contracting-out, franchising, training (Patouillard, Goodman, Hanson & Mills, 2007), and health service delivery (Dewan et al 2006; Newell et al 2005; Balasubramanian et al 2006; Boyle, 1998; Lonnroth et al 2004). 5 Public-Private Partnerships for Healthy Eating Information Gaps Although PPPs in public health are not a new development, research on PPPs with the food industry is still an emerging topic. Most of the literature is focused on large manufacturers who process foods high in sugar, fat and/or sodium. This discussion paper acknowledges that the food industry is made up of growers, producers, manufactures, distributors, retailers and their associations
that vary in size and represent a range of roles, interests and motivations. However, research on growers/producers and retailers regarding PPPs in public health is very limited and the specific benefits and challenges of working with this sector have not been fully examined. Many of the risks and challenges associated with manufactures of processed food may not apply to all companies within the food industry. Examples of initiatives involving the food industry and the government to promote healthy eating are emerging in the literature (Kraak & Story, 2010), although key information related to shared decision-making, resources and expertise are not provided. This limits the understanding of whether those initiatives are actual partnerships or another form of engagement. The literature on PPPs for healthy eating is very limited and refers to a wide variety of interactions and forms of engagement (not necessarily partnerships)(De Pinho, 2012). Hawkes and Buse examined existing
European examples of partnerships between the government and the food industry and found that the term ‘partnership’ was used generically. This created misleading expectations of the partnerships and a shared decision-making power among partner organizations was not evident in the partnership (Hawkes & Buse, 2011). Examples of PPPs for healthy eating come mostly from Europe and a few from the US. These PPPs involve some form of participation of the government and the food industry through the provision of funding, technical expertise, management/ leadership or a combination of these. Some are funded by the government, others by the industry and others jointly; some are initiated by the government, others by industry; some are led by the public sector, others by the food industry; and some involve large multinational companies (Hawkes & Buse, 2011). These partnerships also differ in their purpose and activities, both of which fall into five broad categories: public education
and information, product reformulation, research, access to healthy foods, and platform for discussion (Hawkes, 2008; Hawkes & Buse, 2011). Public education and information includes partnerships for diet and nutrition skills, training, healthy-eating messages and nutrition labeling. Product reformulation often refers to partnerships for sodium reduction in food products, when the PPPs are public-led, or expansion to healthier products, when the PPPs are private-led. PPPs for research bring together food or beverage companies, academia, and public research-funding agencies to support research in the areas of food and health. Partnerships for access to healthy foods refer to access of fruit, vegetables and other healthy food products in underserved communities. Moreover, partnerships as a platform for discussions between the government and industry is a mechanism for developing recommendations, guidelines, and advice or strategies related to food, diet and health (e.g marketing of
food to children) (Hawkes, 2008; Agurto, Rodriguez & Zacarias, 2011) Although not explicitly framed as a public-private partnership, the Canadian government’s Sodium Working Group has been cited as an example of a platform for discussion (between the public and private sectors) whose aim is to facilitate a voluntary reduction of sodium levels in processed food products and foods sold in foodservices establishments (Health Canada, 2010). Hawkes and Buse found that the dominant characteristics of PPPs for obesity prevention were funding arrangements (e.g funding flowing from one to another organization), platform for discussions among partners (eg the development of the food and nutrition strategy in Finland), and organizational structures involving representatives of the public and the private sectors to manage cooperation between these two sectors (Hawkes & Buse, 2011). 6 Risks and Challenges Encountering challenges is inherent to the process of partnership engagement.
The greatest challenge for government in engaging with the private sector is the alignment with and focus on public health goals while avoiding any real or perceived conflict of interest. Throughout the literature, scholars have pointed out considerable scepticism about the motives of the private sector in partnering with the public sector (Reich, 2000). Much of the criticism is concerned with motives of private firms using the partnership as a mechanism to achieve profits, or influencing the agenda of intergovernmental organizations (influencing tax reduction for financial reasons), or even obtaining subsidized public funds for new products (Richter, 2004; Reich, 2000). These concerns have lead researchers to believe that, PPPs could undermine the roles and responsibilities of public institutions in society, leading to distortion of national policies and public-health funding (Buse & Walt, 2000). “The greatest challenge for government in engaging with the private sector is the
alignment with and focus on public health goals while avoiding any real or perceived conflict of interest.” In the case of promoting healthy eating, some companies within the food industry, in particular those who manufacture foods high in fat, sugar and/or sodium, are positioning themselves as part of the obesity solution through efforts such as self-regulation and collaboration with public health organizations and governments (Lewin, Lindstorm and Nestle, 2006). However, research has linked highly processed food and beverages with obesity and other chronic diseases which makes it important to understand the implications of collaborating with this segment of food industry before doing so (Moodie, Stuckler, Monteiro, et al., 2013; Gilmore, Savell and Collin, 2011) A review of literature (not authored or sponsored by industry) found no evidence to support effectiveness or safety of food industry self-regulation or public-private partnerships with “highly processed” food industry
to improve public health (Moodie et al., 2013; Lewin et al, 2006) Most research cautions against working with the “highly processed” food industry for the purpose of public health for several reasons. Although industries strongly assert that self-regulation is sufficient to protect the public, there is no enforcement of third party monitoring of their effects (Lewin et al, 2006) and researchers assert that they may be self-serving, stall other potential government action, and protect “business as usual” (Moodie et al., 2013; Sharma, Teret and Brownell, 2010; Brownell & Warner, 2009) Similarly, companies have modified product formulas and promised to shift marketing efforts toward more nutritious products, while continuing to make and promote less nutritious versions (Moodie et al., 2013; Lewin et al, 2006) Following their review of processed food company promises versus practice, Lewin and colleagues (2006) state that for business reasons alone, these companies cannot –
and will not – stop making and marketing nutritionally questionable food products to children. Sharma and colleagues state that food industry self-regulation may only succeed “with public health input in the planning and execution of regulations, transparency in creating standards, and external, objective evaluation of impact” (Sharma et al, 2010). 7 There is an inherent conflict of interest between public health goals and that of “highly processed” food industry due their legal responsibility to make a profit to return to investors (Wiist, 2011). More specifically, some stipulate that the highly processed food industry has two basic strategic options to enhance shareholder revenue: 1) persuade consumers to eat more; or 2) increase profit margins, especially by marketing reformulated or repackaged products (Ludwig & Nestle, 2008). And since much higher profits come from processed foods compared to fresh foods, advising people to eat less or more healthily contradicts
the core business models of food companies (Ludwig & Nestle, 2008). There are other, less obvious risks to partnering with “highly processed” food industry. Literature states that food industry often uses similar tactics as tobacco to build relationships with public health organizations by promising to self-regulate and/or funding public health initiatives in order to gain influence at the public health table and undermine more effective public health action that would affect their bottom line (Moodie et al., 2013; Gilmore et al, 2011; Koplan & Brownell, 2010; Brownell & Warner, 2009; Ludwig & Nestle, 2008; Lexchin, Bero, Djulbegovic, & Clark, 2003). “Most researchers caution public health professionals and organizations to be aware that corporate enticements of partnerships and funding can blur or disguise the distinction between these differing purposes, goals and values .” Studies also suggest that food industry has an “especially insidious
influence” on the conduct of research and development of public health policy (Ludwig & Nestle, 2008) and challenging the integrity of research that challenges their bottom line (Moodie et al., 2013; Tereskerz, Hamric, Uterbock, & Moreno, 2009; Gilmore et al, 2011) Overall, there is a risk of perceived loss of integrity of a public health organization when associated with “highly processed” food industry who market products that directly conflict with public health recommendations (e.g high in fat, sugar, sodium). Food companies often pressure health organizations to enter cause-related marketing relationships, offering the appeal of leveraging these companies’ broad reach to public health organizations with limited resources. The results may undermine the credibility of these public health organizations and may facilitate access to companies to enhance the marketing of energy-dense products by association with trusted health organizations (Kraak, Kumanyika & Story,
2009). Research warns when favourable nutrition information and/or health claims are presented on products, consumers have more favourable attitudes, including nutrition attitudes, and purchase intentions towards the product (Kozup, Kreyer & Burton, 2003). Furthermore, some have questioned whether industry should be entrusted to convey public health messages by using advertising as a solution to address a problem attributed to excessive advertising (Schor & Ford, 2007). 8 Although research shows that exclusive focus on physical activity is insufficient to offset excess energy consumption associated with marketing practices that promote unhealthy diets (Ludwig & Nestle, 2008) it is increasingly common for “highly processed” food industry to deflect negative attention from processed foods and sugar-sweetened beverages by focusing resources and marketing on physical activity, “implicitly de-emphasizing the role of food quality and portion size in reducing obesity
risk” and placing sole responsibility on the individual (Kraak, Kumanyika, & Story, 2009; Lewin et al., 2006; Koplan & Brownell, 2010). Some literature therefore cautions against cobranding with these companies in an effort to eliminate contradictions in both explicit and implicit healthy lifestyle messages children receive around food and activity choice (Hesketh, Waters, Green, Salmon & Williams, 2005). Intrinsically, the purpose, goal and values of public health and that of processed food corporations are fundamentally different. Most researchers caution public health professionals and organizations to be aware that corporate enticements of partnerships and funding can blur or disguise the distinction between these differing purposes, goals and values (Moodie et al., 2013; Wiist, 2011; Ludwig & Nestle, 2008; Brownell & Warner, 2009). Of further concern is that at the end of the day, “when public health and corporate goals conflict, corporate profit
imperatives often trump public health imperatives” (Lewin et al., 2006) 9 Benefits Experiences Across Canada A survey was conducted to capture experiences, interests and challenges faced across Canada in developing PPPs with the food industry. According to the survey, retailers represented by grocery stores, convenience stores and farmers’ markets seem to be “the most popular” food sector to engage with. Partnerships seem most likely to happen with retailers, often to promote healthy food at point-ofpurchase, followed closely by growers (e.g fruit and vegetables) and producers (eg milk, eggs). Most jurisdictions who responded to the survey indicated that they were interested in developing a national framework and/or sharing information, knowledge and expertise on PPPs with the food industry. For example, one jurisdiction mentioned that the “food industry is multi-national and affects most Canadian jurisdictions” and that by working together, we would have “stronger
influence”. A national dialogue on how to engage with the food industry will allow jurisdictions to capitalize on the expertise and knowledge of other jurisdictions and provide guidance to help governments address the challenges and risks involved in public-private partnerships. See Appendix 1 for more detail. 10 The food industry has made some voluntary attempts to introduce or reformulate existing products to promote healthier choices (Swinburn, Sacks & Hall, 2011; Gortmaker, Swinburn & Levy, 2011; WHO, 2004). The primary motivation might not be to promote better nutrition or to reduce dietary risks. It may simply reflect the recognition that nutrition and dietary issues will continue to be of concern to many governments, researchers, international organizations, professional organizations, advocacy groups and consumers (Cash, 2006; Popkin, 2009). For example, PepsiCo through its subsidiary Frito-Lay has eliminated trans-fats from its salty snacks and developed some
baked-snack options (Cash, 2006). Danone, a global producer of bottled water products, has reduced the sugar content in its sweetened water by 40 percent (compared to its original calorie value) in six countries. Others companies, such as Kraft, Nestle, Unilever have also worked on reducing calories and added sugar in many of their products (Popkin, 2009). In Canada, Loblaw’s introduced the PC Blue Menu Line with the aim of making healthier eating easy and affordable. This line now contains more than 400 products with at least one of the following health benefits: lower fat, lower calories, high fibre, omega-3, soy protein, and lower sodium (Loblaws, 2008). Despite the importance of these measures, the food industry is not eliminating the “unhealthy” food products of their line to truly alter dietary behaviours at a population level (Popkin, 2009). Although it is still not known whether these voluntary measures will promote health benefits at a population level, the reformulation
of these products have resulted in healthier choices (e.g less sugar or less sodium) (De Pinho, 2012). Until recently, the role of the private sector in public health has been viewed with “antagonism, suspicion, confrontation” (Lucas, 2002) by many actors in the field. Governments and inter-governmental organizations are now recognizing that it is necessary to involve multiple stakeholders, including the private sector in the pursuit of a healthy and sustainable society (Rowitz, 2006; WHO, 2004). This recognition has been accompanied with a reassessment of the roles, strengths and limitations of the public sector, the private sector and the civil society in responding to health problems (Widdus, 2001). Proponents of PPPs for public health argue that this form of collaboration has become compelling in an environment of complex health problems (Widdus, 2001), tremendous community need and competition for limited resources (Reich et al, 2003). This is an environment in which neither
side can on its own achieve its specific goals (Lucas, 2002). According to Widdus, partnerships seem to be most justifiable when traditional ways of working independently have a limited impact on a problem, the specific desired goals can be agreed by the collaborating players, complementary expertise is interchanged between both sectors, the long-term interests of each sector are fulfilled (i.e there are benefits to all players involved) and contributions of expertise and resources are reasonably balanced (Widdus, 2001). Whether strategies for obesity prevention are based on increasing physical activity or promoting healthy eating or on both, the strategies cannot be seen as the sole responsibility of one sector (WHO, 2000). The Lancet’s series on obesity prevention suggests that the obesity epidemic is driven by complex forces that require a systems approach to reverse the obese epidemic, further suggesting that strategies be multisectoral and involve the active participation of
governments and the food industry (Gortmaker et al, 2011; WHO, 2000). Governments are important actors in reversing the obesity epidemic, because protection and promotion of public health is a core responsibility of government (Gortmaker et al, 2011). The food industry is also a significant player due to its role in producing, distributing and providing food products Governments around the world have allocated this role to the private sector and allowed companies to generate economic activity from food, which is a product essential for public life and health (Hawkes and Buse, 2011). The Global Strategy on Diet, Physical Activity and Health by the WHO suggests that the private sector become partners with governments to facilitate and enable integrated efforts to encourage healthier environments (WHO, 2004). The shared responsibilities and partnerships between the public and private sector allows for multiple strategies for the prevention and management of obesity (WHO, 2000) and
multifaceted solutions that cut across sectors (Gortmaker et al 2011). To reduce obesogenic environments, which is defined as “the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations” (Lake, 2006: 262), a multi-sectoral approach that mobilizes the combined energy, resources and expertise of all actors is essential for sustained progress. This collective power can achieve sustainable change (Gortmaker et al, 2011; WHO 2003) in a number of core activity areas, including: 1. Health Promotion and communication campaigns (e.g information leaflets and posters); 2. Diet and nutrition education in formal and informal leaning venues (e.g building cooking skills); 3. Communicating information on food products (eg nutrition labeling and healthy food logos); 4. Controlling advertising and marketing of food products (eg advertising codes on marketing); 5. Increasing or decreasing access to food products (eg
fruits and vegetables, vending machines); 6. Conducting or supporting research (eg on development of novel foods); 7. Developing or reformulating food products (eg reducing sodium); 8. Developing recommendations, guidelines, advice, and strategies for governments and industry (e.g government forum that includes the food industry); 9. Encouraging private sector action in general, such as providing a forum for commitments (eg platforms); and, 10. Funding for above activities connected to healthy eating (Hawkes and Buse, 2001: 7). Some scholars claim that PPPs can bring meaningful social changes in the promotion of physical activity and healthful eating (Kraak & Story, 2010). In their view, PPPs should prioritize policies with a broader population-based approach rather than those policies focused on individual behavioural approaches. Other scholars go further in claiming that if properly designed, PPPs for obesity prevention can expedite the adoption of new rules that apply to a wide
range of competing companies (Huang & Yaroch, 2009). If well developed, PPPs with the food industry may offer several advantages for governments to make progress in these areas and provide other benefits (De Pinho, 2012), such as: Better understanding of each other; Collaborative rather than confrontational approach (food industry might be willing to comply with government’s interventions); Innovative mechanism to address societal problem; Leverage food industry expertise; Leverage food industry resources; Provide access to industry data, information, and expertise for research and evaluation (e.g sales data); and Influence food industry practice towards healthy eating. 11 Key Considerations Due to the broad spectrum of potential partners for PPPs to increase public health, it is important to acknowledge that PPPs involve different types of engagement and activities (Hawkes & Buse, 2011). This is especially evident when referring to food
industry given the diversity of segments (i.e, manufactures, producers, retailers, restaurant services) For example, an engagement with food retailers on health messaging is very different from a research collaboration or a forum for discussing reducing marketing to children with manufacturers. No clear guidelines and governance structures exist to guide public health organizations’ decisions on whether and how to engage effectively and efficiently with the food industry (Hawkes & Buse, 2011). A comprehensive but flexible tool is needed in order to: 1) Determine whether private sector engagement would help advance the public health goals and, if so, set criteria for private sector engagement; 2) Define the type of engagement activity; 3) Identify shared goals and possible conflicts of interest; 4) Assess the influence of potential private partners on public health research and policy; and 5) Establish a good governance structure. First, it is important to set criteria for private
sector engagement. Some claim that the current reality is one where public-private collaborations have assumed a role in the exercise of power that affect decisions about how to address chronic diseases and their modifiable factors, like healthy eating (Hawkes & Buse, 2011). In order to ensure that partnerships will advance public health goals and avoid conflict or interest or lost integrity, academics and some in the public health field are calling for clear guidelines to assist organizations to clarify the purpose, terms and management of private-sector engagement. In the context of healthy eating, Hawkes (2011) urges that “it is only after the public health objective has been set that policy makers should even think about engaging with the food industry”. This does not mean there can be no engagement, but Hawkes (2011) suggests only doing so after answering these three questions: 1. Would engaging with food industry help achieve the objective faster and more effectively? 2.
Would the interests involved (on both sides) enhance or threaten the likelihood of achieving the specific objective as well as longer-term public health objectives? 3. If interaction is a viable option, what form of engagement would most effectively achieve the objective while accounting for the different interests: a real partnership or less formal type of collaboration? It is crucial that the partnership or collaboration only be initiated if it will help advance the public health goal, and that the partnership itself it not seen as the outcome (Nishtar, 2004). With the public health goal paramount, not partnering or disengaging is always an option, and sometimes the better one, since “incompatible and poorly executed partnerships can damage public trust, credibility and all partners’ brand reputations” (Kraak et al., 2011) along with potentially causing more harm to public health than not undertaking the initiative in the first place (Brady & Rundall, 2011; Hawkes &
Buse, 2011; Brownell, 2012). 12 Second, it is important to distinguish between a partnership and the broader term of ‘collaboration’, and whether there is a responsible way to engage with the food industry. Some experts believe that collaboration may work if strict criteria are established and a risk analysis is conducted at the outset, transparency and accountability mechanisms are firmly established, and any decision to collaborate is based solely on the ultimate public health objective (Kraak et al., 2009) The term Info graphic: Who owns what in the food industry? (Source: Fritz Kreiss/Occupy Monsanto) “partnership” in the literature refers to anything from education campaigns to joint research activities and may involve a range of processes and structures. But as Hawkes writes: There is an important distinction that can be made: interactions characterized by ‘shared decision-making power among partners’ and those characterized simply by ‘participation’ from
both sectors. In the former, both sectors play a role in decisions about the agenda, goals, strategies, resources, roles and responsibilities of the initiative; in the latter, there may be mutual support, but no shared decision-making. The distinction between ‘partnership’-based and ‘participation’-based initiatives may appear academic and even immaterial given that influence in decision-making can be exerted in the absence of formal structures for decision-making. Still, making the distinction is critical. For a start, using the term ‘partnership’ imprecisely can create misleading expectations For example, a public sector-led initiative may embrace private sector actors as ‘partners’ even when its only interest is gaining private sector concessions or funding with few or no conditions. But by giving the impression to the private sector that it is a real ‘partner’, the public sector is, like it or not, inviting for-profit actors to use the arrangement to serve their
own private sector interests If public health officials want to draw on the potential power of civil society to serve their interests, they would be advised to be clearer about when they need civil society ‘participation’ in an initiative, or actual ‘partners’ (Hawkes and Buse, 2011: 400-01). It is crucial to distinguish the type of engagement a public health organization aims to enter with industry. For example, ‘partnership’ is appropriate when the interaction involves both sectors having a voice in decision-making. If decision making is not shared, terms like ‘interaction’ or ‘engagement’ should be used in order to be clear (Hawkes & Buse, 2011) Third, researchers have identified shared goals and possible conflicts of interest as an imperative consideration when engaging in PPPs. The key to the effectiveness of these relationships is the avoidance of conflict of interest (Kraak et al 2011; Kraak and Story, 2010). If the public health goals and those of the
industry collaborator do not conflict, there is potential for an effective collaboration Avoiding conflict of interest is challenging when choosing food industry collaborators to prevent obesity or promote healthy eating due to inherent business objectives of some segments of the industry (Wiist, 2011; Gilmore et al., 2011) However, the concept of shared goals and working with other private sector collaborators with whom there is no potential conflict of interest could hold promise 13 Fourth, governments need to consider the influence of the private sector over research and public health policy. Lesser et al (2007) analyzed 206 nutrition-related scientific articles published over a 5-year period that addressed the health effects of milk, fruit, juices, and soft drinks. The likelihood of a conclusion favourable to the financial interests of the sponsoring company was 4fold to 8-fold higher if the study received full rather than no industry funding, pointing to a systematic bias.
Food companies also donate large sums of money to professional associations in order to receive “a national platform via events and programs with prominent access to key influencers, thought leaders and decision makers” (Ludwig and Nestle, 2008) in an attempt to “gain a seat” at in those forums and influence public health policy (Moodie et al., 2013; Lexchin et al, 2003; Gilmore et al, 2011; Koplan & Brownell, 2010) For example, 10 of 12 partners and sponsors of the American Academy of Nutrition and Dietetics are processed food companies (Academy of Nutrition and Dietetics’ website, 2013). In a recent report, public health attorney and author Michele Simon claimed that this undermines the integrity of those professionals most responsible for educating Americans about healthy eating (Simon, 2013). Throughout the literature, there is considerable evidence that companies use tactics to undermine public health taxation and regulations (Stuckler and Nestle, 2012) and deflect
criticisms of their core practices by introducing and promoting healthier processed foods (Brownell, 2012 and Moodie et al, 2013). “A well designed and executed partnership can support transformative systems change while an incompatible and poorly executed one can damage public trust and the credibility of all partners.” Lastly, to maximize benefits and minimize risks, good governance structures are required to support government collaboration with the food industry. There is a governance gap and no clear structure in place to enable governments to engage with the food industry to promote healthy eating (Hawkes and Buse, 2011). This makes it important to establish formal governance structures when collaborating with private partners. The type of engagement and kind of activity to be undertaken must be considered as different skills, functions, resources, roles and responsibilities are required. Any identified risks should also be addressed within the governance structure as it is
designed (Hawkes and Buse, 2011). Accountability processes should be developed within the governance structure to balance private and public health interests, manage conflicts of interest, ensure co-branded activities support healthy products and healthy eating environments, comply with ethical codes of conduct, assess partnership compatibility and monitor partnership outcomes (Kraak et al, 2011). Given the risks involved for both public and private partners, a process to disengage and dissolve a partnership should be established within the governance structure. A well designed and executed partnership can support transformative systems change while an incompatible and poorly executed one can damage public trust and the credibility of all partners (Kraak et al, 2011). 14 Conclusion Encountering challenges is inherent to the process of deciding whether to develop PPPs with the food industry. In order to overcome these challenges, governments need to consider a number of issues
before pursuing engagement opportunities. It is important to be clear on underlying goals of potential partners and determine whether: 1) collaboration will advance short and long-term public health goals, 2) what type of engagement activity is most effective (e.g platform for discussion, alliance, partnership), and 3) the goals of the potential collaborator are not in conflict with the public health objective. A number of jurisdictions across Canada are already engaged in PPPs with food industry and have expressed interest in a national dialogue on this issue. This paper will support that dialogue and is the first step in developing a national framework on how to engage with the food industry. 15 Appendix 1: Interest and Experience across Canada In addition to completing a literature review, a brief survey was conducted to capture experiences, interests and challenges faced across Canada in developing PPPs with the food industry. In November 2012, the Public Health Agency of
Canada circulated the survey to all 13 provinces and territories. Eight out of 13 jurisdictions responded the survey. Six jurisdictions reported that they have engaged with the food industry and seven reported that they are very interested or interested in exploring options for partnerships with the food industry. Among the six jurisdictions that have engaged with the food industry, all of them have entered into a partnership model, and more than half have engaged in a “platform for discussion” created for information sharing. The majority of jurisdictions have also engaged in lower levels of engagement through donation or sponsorship Jurisdictions have reported multiple types of engagement with the food industry and are approaching the full spectrum of the food sector ranging from producers to retailers. According to the survey, retailers represented by grocery stores, convenience stores and farmers’ markets seem to be “the most popular” food sector to engage with.
Partnerships seem most likely to happen with retailers, often to promote healthy food at point-of-purchase, followed closely by growers (e.g fruit and vegetables) and producers (e.g milk, eggs) Each jurisdiction was asked to rank which type of partnership would be most relevant to their jurisdiction. Partnerships to increase access to healthy foods (eg fruit and vegetables) were viewed as the most relevant type of partnership to develop with the food industry, followed by partnerships for public education and information (e.g promotion of healthy-eating messages, food skills, etc) These two types of partnerships do not seem to be mutually exclusive, as public education and information approaches can be used to promote access to healthy foods. In any partnership, partners expect to obtain certain benefits as the result of the engagement. It was interesting that jurisdictions across Canada expect, as the most important benefit, to influence food industry practices to promote healthy
eating while leveraging food industry resources (e.g financial, human and physical resources) and their ability to “get the message out” efficiently Jurisdictions also acknowledged that the most appropriate role for the government in a PPP with the food industry is to build trust among partner organizations and provide leadership in the overall partnership. These aspects are also reported in other examples of PPPs for public health (e.g PPPs with pharmaceutical companies, partnerships with private health providers). Research indicates that there is still considerable skepticism about the motives of the private sector in partnering with the public sector. This skepticism can undermine any attempt to overcome mistrust among partner organizations and create an environment for collaboration. Building trust among partner organization is an essential step in the process of developing a PPP (De Pinho, 2012). The question is how to make the most of the food industry’s role and expertise
to prevent obesity presents numerous challenges. Conflicting values (often explained by the profit motives vs. public health goals) and the perceived co-option of publichealth goals by commercial interest were identified by jurisdictions as the most risky aspects of engaging with the food industry. Scholars have suggested that partner organizations adopt systematic and transparent accountability processes in order to maximize the benefits and reduce these types of risks. For example: 16 Managing conflict of interest and bias in decision making; Ensuring that co-branded activities support healthy products and healthy eating; Complying with ethical codes of conduct; Undertaking due diligence to assess partnerships; and, Monitoring and evaluating partnership outcomes. Government priorities seem to determine whether a jurisdiction decides to enter into a partnership with the food industry, followed by having a previous or existing relationship with the food
industry. Jurisdictions that had not engaged with the food industry provided reasons related to conflicting values/goals between the public and the privates sectors, concerns about public perception and limited organizational capacity to build these partnerships. Jurisdictions with previous experience in engaging with the food industry reported similar challenges (e.g mistrust of industries to partner with the government; different priorities among partner organizations, etc.) Other challenges included: finding an appropriate partner for effective partnerships; the need for a champion to facilitate access to industry partners; appropriate measures for monitoring the purchase and consumption of healthy food; the need to ‘recognize’ the efforts and achievements of the food industry; and, the need to ensure program sustainability. At the same time, jurisdictions reported positive outcomes, such as: Increased awareness and demand for local foods by establishing venues for
dialogue with consumers about topics associated with food (e.g food preparation); Interest from the food and beverage industry in supporting healthy eating programs such as school healthy eating policies; and Increased availability and accessibility to foods such as fruit and vegetables by increasing investments in local food infrastructure and partnership development with the food industry and promotion of healthy food at pointof-purchase. Jurisdictions also reported a number of lessons learned, such as: Making initiatives voluntary but “irresistible”; Maximizing linkages with other partners and programs; Maintaining communication is essential; and Having leadership at the federal level is required to support consistent messaging regarding healthy eating and PPPs. Most jurisdictions who responded to the survey indicated that they were interested in developing a national framework and/or sharing information, knowledge and expertise on PPPs with the food industry.
For example, one jurisdiction mentioned that the “food industry is multi-national and affects most Canadian jurisdictions” and that by working together, we would have “stronger influence”. A national dialogue on how to engage with the food industry will allow jurisdictions to capitalize on the expertise and knowledge of other jurisdictions and provide guidance to help governments address the challenges and risks involved in public-private partnerships. 17 Reference List Academy of Nutrition and Dietetics. Who are the Academy’s Corporate Sponsors: http://wwweatrightorg/ corporatesponsors/ (retrieved March 2013). Agurto I, Rodriguez L, Zacarias I. (2011) Food and vegetable promotion and the 5-a-day programme in Chile for the prevention of chronic non-communicable diseases: across-sector relationships and public-private partnerships. In: Blas E, Sommerfeld J, Sivasankara Kurup A (eds.) Social Determinants Approaches to Public Health: from concept to practice World Health
Organization: Geneva 2011 Asante AD, Zwi AB. (2007) Public-private partnerships and global health equity: prospects and challenges Indian Journal of Medical Ethics, 4, 176-80 Balasubramanian R, Rajeswari R, Vijayabhaskara RD, Jaggarajamma K, Gopi PG, Chandrasekaran V, et al. (2006) A rural public-private partnership model in tuberculosis control in South India. International Journal of Tuberculosis and Lung Disease, 10, 1380-85. Boyle DP, Gardner J, Callaway J. (1998) A partial hospitalization program provided through a public-private partnership Clinical gerontologist, 19, 21-37 Brady, M., & Rundall, P Governments should govern, and corporations should follow the rules SCN News 2011, 39, 51 -56. Bravo NR. (2007)The challenge for NIH ethics policies: preserving public trust and biomedical progress Cleveland Clinic journal of medicine, 74, S29-31 Brownell, K.D, Kersh, R, Ludwig, DS, Post, RC, Puhl, RM, Schwartz, MB & Willett, WC (2010) Personal Responsibility and Obesity: A
Constructive Approach to a Controversial Issue Health Affairs, 29(3), 379-387 Brownell, K.D, & Warner, KE (2009) The Perils of Ignoring History: Big Tobacco Played Dirty and Millions Died How Similar is Big Food? The Milbank Quarterly, 87(1), 259-294. Brownell, K.D (2012) Thinking forward: The quicksand of appeasing the food industry PLoS, 9(7), e10001254 Buse K, Walt G. (2000) Global public-private partnerships: part II - what are the health issues for global governance? Bulletin of the World Health Organization, 78, 699-709. Buse K, Waxman A. (2001) Public-private health partnerships: a strategy for WHO Bulletin of the World Health Organization, 79, 748-54 Cash SB, Goddard EW, Lerohl M. (2006) Canadian Health and Food: The links between Policy, Consumers and Industry Canadian Journal of Agricultural Economics, 54, 605-29. Clasen TF. (2002) The public-private partnership for the Central American hand washing initiative: reflections from a private sector perspective. Tropical
Medicine & International Health, 7, 197-200 De Pinho Campos, K. (2012) Public-Private Partnerships for Obesity Prevention Paper prepared for the qualifying examination of the doctoral program in the Dalla Lana School of Public Health, University of Toronto (unpublished) De Pinho Campos , K., Norman, CD, Jadad, AR (2011) Product development public-private partnerships for public health: A systematic review using qualitative data. Social science & medicine, 73, 986-94 Dewan, P.K, Lal, SS, Lonnroth, K, Wares, F, Uplekar, M, & Sahu, S, et al (2006) Improving tuberculosis control through public-private collaboration in India: literature review. BMJ, 332, 574-78 Field JE, Peck E. (2003) Public-private partnerships in healthcare: the managers perspective Health & Social Care in the Community, 11, 494-501. Gilmore, A.B, Savell, E, & Collin, J (2011) Editorial: Public health, corporations and the new responsibility deal: promoting partnerships with vectors of disease?
Journal of Public Health 33(1), 2-4 18 Gortmaker, S.L, Swinburn, BA, Levy, D, Carter, R, Mabry, PL, Finegood, DT, Huang, T, March, T, & Moodie, M (2011). Changing the future of obesity: science, policy, and action Lancet,378, 838-847 Hardon A. (2006) Immunisation for all?: A critical look at the first GAVI partners meeting HAI Europe, 6 (1), 2-9 Hawkes, C. (2004) Marketing Food to Children: the Global Regulatory Environment Geneva: World Health Organization; http://whqlibdoc.whoint/publications/zoo4/9241I591579pdf (Retrieved March 2013) Hawkes C. (2008) Working Paper on Public-Private Partnerships for Health High Level Group - Working Paper European Commission 2008. Hawkes C, Buse K. (2011) Public health sector and food industry interaction: its time to clarify the term partnership‚ and be honest about underlying interests. The European Journal of Public Health, 21, 400-01 Hawkes C, Buse K. Public-Private Engagement For Diet and Health: Addressing the Governance Gap SCN News
2011; 39: 6-10. Hesketh, K., Waters, E, Green, J, Salmon, L, & Williams, J (2005) Healthy eating, activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion International, 20(1), 19-26 Huang TT, Yaroch AL. (2009) A public-private partnership model for obesity prevention Preventing Chronic Disease, 6 (3), 1-2. Huxham C, Vangen S, Huxham C, Eden C. (2000) The Challenge of Collaborative Governance Public Management Review, 2, 337-57 Kickbusch I, Lister G. (2006) Europe must establish a societal dialogue for global health: Public-private partnership European Perspective on Global Health: A policy glossary European Foundation Centre: Brussels, Belgium 2006 Koplan, J.P, & Brownell, KD (2010) Response of the Food and Beverage Industry to the Obesity Threat JAMA 304(13), 1487-1488. Kozup, J.C, Kreyer, E H, & Burton, S (2003) Making Healthful Food Choices: The Influence of Health Claims and Nutrition Information on Consumers
Evaluations of Packaged Food Products and Restaurant Menu Items Journal of Marketing 67(2), 19-34 Kraak VI, Kumanyika SK, Story M. (2009) The commercial marketing of healthy lifestyles to address the global child and adolescent obesity pandemic: prospects, pitfalls and priorities. Public Health Nutrition, 2009, 12, 2027-36 Kraak VI, Story M. (2010) A public health perspective on healthy lifestyles and public-private partnerships for global childhood obesity prevention. Journal of the American Dietetic Association, 110, 192-200 Kraak VI, Swinburn BA, Lawrence JM, Harrison P. (2011) The Accountability of Public-Private Partnership with Food, Beverage and Quick-Serve Restaurant Companies to Address Global, Hunger, and the Double Burden of Malnutrition. SCN News, 39, 11-22. Lake, A. (2006) Obesogenic environments: exploring the built and food environments The Journal of The Royal Society for the Promotion of Health, 126(6), 262-267. Lesser, L.I, Ebbeling, CB, Goozner, M, Wypij, D, &
Ludwig, DS (2007) Relationship between funding source and conclusion among nutrition-related scientific articles PLoS Med, 4(1), e5 Levine OS, Cherian T, Shah R, Batson A. (2004) PneumoADIP: An example of translational research to accelerate pneumococcal vaccination in developing countries Journal of Health, Population and Nutrition, 22, 268-74 Lewin A, Lindstrom L, Nestle M. (2006) Food Industry Promises to Address Childhood Obesity: Preliminary Evaluation Journal of Public Health Policy, 27, 327-454. Lexchin, J., Bero, LA, Djulbegovic, B, & Clark, O (2003) Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ, 326, 1160-1170 Loblaw. (2008) The Way We Do Business Corporate Social Responsibility Report Loblaw Companies Limited 19 Lonnroth K, Uplekar M, Arora VK, Juvekar S, Lan NTN, Mwaniki D, et al. (2004) Public-private mix for DOTS implementation: what makes it work? Bulletin of the World Health Organization, 82, 580-86 Lucas AO.
Public-Private Partnerships: Ilustrative Examples In: Reich MR (ed) (2002) Public-Private Partnerships for Public Health. Harvard University Press: Cambridge, MA 2002 Ludwig, D.S, & Nestle, M (2008) Can the Food Industry play a constructive role in the obesity epidemic? J am Med Assoc, 300, 1808-1811. Meredith S, Ziemba E. (2007) A new landscape of partnerships Global Forum Update on Research for Health: Equitable Access: Research challenges for health in developing countries Global Forum for Health Research: Geneva, Switzerland 2007 Ministry of Health of Canada. Sodium Reduction Strategy for Canada: Recommendations of the Sodium Working Group. In: Division NE (ed) Ministry of Health of Canada: Ottawa 2010 Mitchell-Weaver C, Manning B. (1991) Public-private partnerships in third world development: A conceptual overview Studies in Comparative International Development (SCID), 26, 45-67 Moodie, R., Stuckler, D, Monteiro, C, Sheron, N, Neal, B, Thamarangsi, T, Lincoln, P, &
Casswell, S (2013) Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. The Lancet, 381(9867), 670–679. http://dxdoiorg/101016/S0140-6736(12)62089-3 (retrieved March 2013) Newell JN, Pande SB, Baral SC, Bam DS, Malla P. (2005) Leadership, management and technical lessons learnt from a successful public-private partnership for TB control in Nepal. International Journal of Tuberculosis and Lung Disease, 9, 1013-17. Nishtar S. (2004) Public-private partnerships in health - A global call to action Health Research Policy and Systems, 2 (5), 1-7. Patouillard E, Goodman CA, Hanson KG, Mills AJ. (2007) Can working with the private for-profit sector improve utilization of quality health services by the poor? A systematic review of the literature International Journal for Equity in Health, 6, 6-17. Peters BG. (1998) With a Little Help From Our Friends: Public-Private Partnerships as Institutions and Instruments In: Pierre J
(ed.) Partnerships in urban governance : European and American experience St Martins Press Inc: New York 1998; 11-33. Popkin BM. (2009) The World Is Fat: The fads, trends, policies, and products that are fattening the human race New York: Penguin Group (USA). Reich, M. R (2000) Public-private partnerships for public health Nature medicine, 6: 617-20 Reich MR. (2002) Public-private partnerships for public health Cambridge, MA: Harvard University Press Reich MR, Hershey JH, Hardy GE, Jr., Childress JF, Bernheim RG (2003) Workshop on public health law and ethics I & II: The challenge of public/private partnerships (PPPs). Journal of Law, Medicine & Ethics, 31 (s4): 90-93 Richter, J. (2004) Public-Private Partnerships for Health: A Trend with no alternatives? Development, 47: 43-48 Ridley RG. (2001) Putting the "partnership" into public-private partnerships WHO Drug Information, 15, 57-58 Rowitz L. (2006) Public Health for the 21st Century: the prepared leader Sudbury,
MA: Jones and Bartlett Publishers, Inc. Schor, J. & Ford, M (2007) From tastes great to cool: children’s food marketing and the rise of the symbolic J Law Med Ethics 35, 10–21. Sharma, L.L, Teret, SP, & Brownell, KD (2010) The Food Industry and Self-Regulation: Standards to Promote Success and to Avoid Public Health Failures. American Journal of Public Health, 100(2), 240-246 20 Simon, M. (2013) Are America’s nutrition professionals in the pocket of Big Food? Eat Drink Politics: http:// www.appetiteforprofitcom/2013/01/22/and-now-a-word-from-our-sponsors-new-report-from-eat-drink-politics/ (retrieved March 2013). Stuckler D, Nestle M. (2012) Big Food, Food Systems, and Global Health PLoS Med 9(6): e1001242 doi:101371/ journal.pmed1001242 Swinson, B.A, Sacks, G, Hall, KD, McPherson, K, Finegood, DT, Moodie, ML, & Gortmaker, SL (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet, 378, 804-814 Tereskerz, P., Hamric, AB,
Uterbock, TM, & Moreno, JD (2009) Prevalence of industry support and its relationship to research integrity. Accountability in Research, 16, 78–105 The Canadian Council for Public-Private Partnerships. Definitions of PPP Toronto 2011; http://wwwpppcouncilca/ resources/about-ppp/definitions.html The Pharmaceutical Security Institute. Partnership for Safe Medicines http://wwwsafemedicinesorg/: 2011 Van Huijstee MM, Francken M, Leroy P. (2007) Partnerships for sustainable development: a review of current literature Environmental Sciences, 4, 75-89 WHO. (2000) Obesity: Preventing and Managing the Global Epidemic, Technical Report Series No 894 Geneva: World Health Organization: http://whqlibdoc.whoint/trs/WHO TRS 894pdf, (retrieved March 2013) WHO. (2002) Health: Marketing and Youth Conference Italy: World Health Organization: http://wwwwhoint/healthmktg/ about conferencehtm (retrieved March 2013) WHO (2003). FAO Diet, Nutrition and the Prevention of Chronic Diseases, Technical
Report Series No 916 Geneva: World Health Organization: http://whqlibdoc.whoint/trs/WHO TRS 9 6pdf (retrieved March 2013) WHO (2004). Global Strategy on Diet, Physical Activity and Health Retrieved from http://wwwwhoint/ dietphysicalactivity/strategy/eb11344/strategy english web.pdf Widdus R.(2005) Public-private partnerships: an overview Transactions of the Royal Society of Tropical Medicine & Hygiene, 99, S1-8 Widdus R. (2001) Public-private partnerships for health: their main targets, their diversity, and their future directions Bulletin of the World Health Organization, 79, 713-20. Wiist, B. (2011) The Risks to Public Health from Partnerships with Corporations Corporations and Health Watch: Tracking the effects of corporate partnerships on health http://corporationsandhealthorg/2011/05/11/the-risks-to-publichealth-from-partnerships-with-corporations/ (retrieved March 2013) Yerby MS. (1998) A north american registry for epilepsy and pregnancy, a unique public/private partnership
of health surveillance. Epilepsia, 39, 793-98 21 Multi-Sectoral Partnership Task Group The mandate of the Task Group is to develop a guiding framework to support jurisdictions to undertake an evidence-informed approach to partnership development with the food industry. This Task Group will be established from March to September 2013 The goals of the Task Group are to: Articulate how PPPs from public health differ from other types of engagements with the private sector; Explore how PPPs for public health are organized and their objectives; Identify key issues when assessing the development of partnerships between the government and the food industry; Discuss mechanisms/tools for the partnership development with the food industry; and Provide examples of empirical PPPs in diet, nutrition and obesity prevention nationally and internationally. 22
jurisdictions have already established partnerships in this area. When industry is involved in public health research and interventions, there is potential for conflicts of interest and an examination of these types of partnerships is warranted. In the absence of policies and guidance documents, governments have identified the need to develop an evidence-based approach to engage with this segment of the private sector. This paper examines the use of PPPs in public health and engaging the food industry on healthy eating. It highlights findings from the literature regarding risks, challenges, benefits and key considerations for governments in the development and use of PPPs in this area. A summary of experiences, interests and challenges faced in jurisdictions across Canada in developing PPPs with the food industry is also provided The overall purpose of this paper is to share knowledge of PPPs with the food industry and support the development of a framework to enable jurisdictions to
undertake an evidence-informed approach to assess partnership development opportunities with the food industry. The framework will also support decision making when exploring partnerships with other private sectors for the purposes of public health. Purpose and Scope In September 2010, Federal-Provincial/Territorial (F-P/T) Ministers of Health and/or Healthy Living/Health Promotion endorsed a Declaration on Prevention and Promotion and committed to making the promotion of health and the prevention of disease, disability and injury a shared priority for action. As the first commitment of the Declaration, Ministers endorsed the Curbing Childhood Obesity: A Federal, Provincial and Territorial Framework for Action to Promote Healthy Weights (Healthy Weights Framework) and committed to working together and with other sectors on joint actions that will help Canadians live longer, healthier lives. In November 2011, all Ministers (except Quebec) released a report entitled Actions Taken and
Future Directions 2011 (Healthy Weights Report). The report proposes recommendations and actions that can be taken by Ministers of Health and their respective governments, as well as other sectors, to advance efforts to curb childhood obesity. “Over the last two decades, PPPs for public health have gained great attention and recognition among the global public health community” Key Terms Public-private partnerships in public health are defined as at least one representatives from government and one from the private-for-profit sector working together to achieve a shared public health objective based on some degree of shared decision-making. The food industry is made up of growers, producers, manufacturers, distributors, retailers and their associations that range in size from smallmedium enterprises to large multi-national corporations. Partnerships on healthy eating cover a range of activities related to healthy weights, obesity prevention, diet and nutrition. 2 The Healthy
Weights Report recognizes the need for all sectors, including the private sector, to work together to address the multiple factors affecting childhood obesity across Canada. There are a number of strategies within the Healthy Weights Framework that governments can collaborate with the private sector on, including: Increasing the availability and accessibility of nutritious food; Decreasing marketing of food and beverages high in fat, sugar and/or sodium to children; and, Improving the physical environment where children live, learn and play to promote physical activity. Over the last two decades, public-private partnerships (PPPs) for public health have gained great attention and recognition among the global public health community as a strategy to potentially overcome barriers that otherwise neither sector could respond to on its own (Widdus, 2005; Reich, Hershey, Hardy, Childress & Bernheim, 2003). Governments have been facing increasing pressure to take action to
prevent and reduce obesity and chronic disease while experiencing fiscal constraints. This has made PPPs an attractive mechanism to collaborate with the private sector to address obesity and chronic disease prevention (De Pinho, 2012). For the purposes of this paper, public-private partnerships in public health are defined as at least one representative from government and one from the private-for-profit sector working together to achieve a shared public health objective based on some degree of shared decision-making. There are a wide range of industries within the private sector that could be engaged to address issues related to healthy eating, including: the food industry (producers, manufacturers, distributors, retailers and associations), health care (insurance and pharmaceuticals), sports and athletics industry Research Methodology (teams, equipment and apparel) and children’s products and entertainments (toys, games, TV and other media). This paper focuses on the food
industry given that access to healthy, nutritious and affordable food is a significant determinant of health. The food industry is made up of growers, producers, manufacturers, distributors, retailers and their associations that range in size from small-medium enterprises to large multi-national corporations. For the purposes of this paper, partnerships on healthy eating cover a range of activities related to healthy weights, obesity prevention, diet and nutrition. This paper will highlight findings from the literature regarding benefits and challenges of engaging with certain segments of the food industry on healthy eating. This discussion paper is based on the findings of two independent literature reviews conducted by Ontario and Health Canada. The review completed by Ontario, examined the literature on PPPs for public health with an emphasis on diet, nutrition and obesity prevention. It examined reasons for engaging in PPPs in public health, contentious issues, engagement models
and barriers to working with industry on obesity prevention. The review completed by Health Canada focused on research regarding benefits and risks of collaborating with the private sector on public health issues. It examined the food industry and several important factors for government to consider before developing these arrangements, such as conflict of interest. Collaborating with the food industry to support healthy eating is a new area of work for government. Policies have been established to address PPPs with other sectors, such as tobacco, alcohol and pharmaceuticals; however, there are no guiding documents in place when it comes to the food industry. Governments have identified the need to develop an evidence-based approach to support their decision-making process in this area. This paper aims to share knowledge of PPPs with the food industry and support a national dialogue on this issue. It is the first step in developing a national framework that will support jurisdictions
to undertake an evidence-informed approach when assessing whether and with whom to partner with to support healthy eating initiatives. It highlights findings from the literature regarding risks, challenges, benefits and key considerations for governments in the development and use of PPPs in this area. Although it is out of scope for this paper, it is recognized that other areas of government (outside of public health) are engaged with the food industry and health/healthy living ministries may want to recommend that a ‘health in all public policy’ approach be adopted. This would limit all government activities with companies in the food industry whose activities conflict with public health goals in the same way governments have restricted activities with tobacco companies. 3 Public-Private Partnerships in Public Health The literature on PPPs for public health lacks a well-grounded conceptualization of the term “public-private partnership”. The term “partnership” is
used loosely with no consensus around its definition (Field & Peck, 2003), is loaded with ambiguities (Asante & Zwi, 2007) and has become a buzzword in the field (Van Huijstee, Francken & Leroy 2007). It is often difficult to distinguish the meaning of partnerships from other forms of cross-organizational activities such as building an alliance, collaborating, cooperating, networking and joint-working (Huxham, Vangen Huxham & Eden, 2000). Within the field of public health, PPPs are described as any form of engagement or interaction between the public and the private sectors (Hawkes, 2008) However, different forms of engagement have varying degrees of complexity and can be placed along a continuum (Table 1). In which case, partnerships appear at the end of the continuum due to their higher complexity and structured, formal arrangements (Rowitz, 2006). Table 1: Forms of Engagement with the Private Sector Donation Charitable financial or in-kind donations that enhance each
partner’s brand image. Platforms for Discussion Sponsorship Alliances Partnerships Platforms for discussion are often created for information sharing. They bring together different actors to map out strategies for addressing changes. Any form of monetary or inkind payment or contribution to an event, activity or individual that promotes a company’s name, brand, products or services. Alliances are groups of organizations that combine forces to address specific public health issues. They create informal agreements to provide programs or services to the community. A partnership is a mechanism based on shared decision-making that brings together a diversity of skills and resources of various organizations in innovative ways to improve specific outcomes. Lower-level of Complexity Higher-level of Complexity There are important elements that distinguish these forms of engagement which influence how it is designed, implemented and evaluated. For example, a “platform for
discussion” is often created to share information and has no formal governance structure. On the other hand, “partnerships” are more formal and encompass a set of key elements, such as: the presence of multiple actors; having shared goals; developing commitments, roles and responsibilities as part of the agreement; a mutually agreed division of resources and expertise; and, a decision-making process negotiated among partner organizations (Ridley, 2001; Buse & Waxman, 2001; Widdus, 2005; Reich, 2000; Peters, 1998; The Canadian Council for Public-Private Partnerships, 2011). 4 Another difficulty with the term PPPs is determining what constitutes the “public” and the “private” sectors (Reich, 2000; Hawkes, 2008; Buse & Walt, 2000; Kickbusch & Lister, 2006). In this paper, the “public sector” refers to any level of government or governmental agency and the “private sector” refers to for-profit organizations, associations representing for-profit
organizations or private foundations (e.g the Bill and Melinda Gates Foundation) Non-profit organizations and inter-governmental agencies, such as the World Health Organization, are considered the third party within PPPs. These differences can be fundamental as they have implications for governance, accountability, values and ethical considerations (De Pinho, 2012) Types of Partnerships in Public Health Public-private partnerships within the public health sector are not a new development and have been taking place since the early 2000s. Within the literature, the predominant form of classification is based on the goals or objectives of the partnership (Reich, 2002) Using a goal oriented classification, the majority of PPPs have been found to cluster into partnerships for disease control, which in turn is split into two categories of partnerships. Firstly, PPPs for product development, which focuses on research and development of drugs, vaccines and new diagnostics, and secondly, PPPs
for access to drug and vaccines, involving the provision of discounted or donated drugs and vaccines (Widdus, 2005). Additionally, PPPs for strengthening health services, (Dewan , Lal, Lonnroth, Wares, Uplekar, Sahu, et al, 2006; Newell, Pande , Baral, Bam, & Malla 2005; Balasubramanian, Rajeswari & Vijayabhaskara et al, 2006; Boyle, Gardner & Callaway 1998; Lonnroth, Uplekar & Arora et al, 2004), improving advocacy and education (Clasen, 2002; Bravo, 2007; Yerby, 1998; Meredith & Ziemba, 2007), improving regulation, quality and standards (The Pharmaceutical Security Institute, 2011) and global financing coordination (Hardon, 2001; Levine, Cherian , Shah & Batson, 2004) are among the subset of goal-oriented PPPs. The organizational structures of PPPs are inherently different as partnerships are considered context specific (De Pinho, 2012). PPPs can be structured in a way that they are legally dependent, not-for-profit organizations, such as Medicine for Malaria
Ventures (MMV) and Global Alliance for Vaccines and Immunization (GAVI) (De Pinho Campos, Norman & Jadad, 2011). Others are less structured and have been designed as informal collaboration between the public and private for-profit health providers in the form of socialmarketing activities, vouchers, pre-packaging, contracting-out, franchising, training (Patouillard, Goodman, Hanson & Mills, 2007), and health service delivery (Dewan et al 2006; Newell et al 2005; Balasubramanian et al 2006; Boyle, 1998; Lonnroth et al 2004). 5 Public-Private Partnerships for Healthy Eating Information Gaps Although PPPs in public health are not a new development, research on PPPs with the food industry is still an emerging topic. Most of the literature is focused on large manufacturers who process foods high in sugar, fat and/or sodium. This discussion paper acknowledges that the food industry is made up of growers, producers, manufactures, distributors, retailers and their associations
that vary in size and represent a range of roles, interests and motivations. However, research on growers/producers and retailers regarding PPPs in public health is very limited and the specific benefits and challenges of working with this sector have not been fully examined. Many of the risks and challenges associated with manufactures of processed food may not apply to all companies within the food industry. Examples of initiatives involving the food industry and the government to promote healthy eating are emerging in the literature (Kraak & Story, 2010), although key information related to shared decision-making, resources and expertise are not provided. This limits the understanding of whether those initiatives are actual partnerships or another form of engagement. The literature on PPPs for healthy eating is very limited and refers to a wide variety of interactions and forms of engagement (not necessarily partnerships)(De Pinho, 2012). Hawkes and Buse examined existing
European examples of partnerships between the government and the food industry and found that the term ‘partnership’ was used generically. This created misleading expectations of the partnerships and a shared decision-making power among partner organizations was not evident in the partnership (Hawkes & Buse, 2011). Examples of PPPs for healthy eating come mostly from Europe and a few from the US. These PPPs involve some form of participation of the government and the food industry through the provision of funding, technical expertise, management/ leadership or a combination of these. Some are funded by the government, others by the industry and others jointly; some are initiated by the government, others by industry; some are led by the public sector, others by the food industry; and some involve large multinational companies (Hawkes & Buse, 2011). These partnerships also differ in their purpose and activities, both of which fall into five broad categories: public education
and information, product reformulation, research, access to healthy foods, and platform for discussion (Hawkes, 2008; Hawkes & Buse, 2011). Public education and information includes partnerships for diet and nutrition skills, training, healthy-eating messages and nutrition labeling. Product reformulation often refers to partnerships for sodium reduction in food products, when the PPPs are public-led, or expansion to healthier products, when the PPPs are private-led. PPPs for research bring together food or beverage companies, academia, and public research-funding agencies to support research in the areas of food and health. Partnerships for access to healthy foods refer to access of fruit, vegetables and other healthy food products in underserved communities. Moreover, partnerships as a platform for discussions between the government and industry is a mechanism for developing recommendations, guidelines, and advice or strategies related to food, diet and health (e.g marketing of
food to children) (Hawkes, 2008; Agurto, Rodriguez & Zacarias, 2011) Although not explicitly framed as a public-private partnership, the Canadian government’s Sodium Working Group has been cited as an example of a platform for discussion (between the public and private sectors) whose aim is to facilitate a voluntary reduction of sodium levels in processed food products and foods sold in foodservices establishments (Health Canada, 2010). Hawkes and Buse found that the dominant characteristics of PPPs for obesity prevention were funding arrangements (e.g funding flowing from one to another organization), platform for discussions among partners (eg the development of the food and nutrition strategy in Finland), and organizational structures involving representatives of the public and the private sectors to manage cooperation between these two sectors (Hawkes & Buse, 2011). 6 Risks and Challenges Encountering challenges is inherent to the process of partnership engagement.
The greatest challenge for government in engaging with the private sector is the alignment with and focus on public health goals while avoiding any real or perceived conflict of interest. Throughout the literature, scholars have pointed out considerable scepticism about the motives of the private sector in partnering with the public sector (Reich, 2000). Much of the criticism is concerned with motives of private firms using the partnership as a mechanism to achieve profits, or influencing the agenda of intergovernmental organizations (influencing tax reduction for financial reasons), or even obtaining subsidized public funds for new products (Richter, 2004; Reich, 2000). These concerns have lead researchers to believe that, PPPs could undermine the roles and responsibilities of public institutions in society, leading to distortion of national policies and public-health funding (Buse & Walt, 2000). “The greatest challenge for government in engaging with the private sector is the
alignment with and focus on public health goals while avoiding any real or perceived conflict of interest.” In the case of promoting healthy eating, some companies within the food industry, in particular those who manufacture foods high in fat, sugar and/or sodium, are positioning themselves as part of the obesity solution through efforts such as self-regulation and collaboration with public health organizations and governments (Lewin, Lindstorm and Nestle, 2006). However, research has linked highly processed food and beverages with obesity and other chronic diseases which makes it important to understand the implications of collaborating with this segment of food industry before doing so (Moodie, Stuckler, Monteiro, et al., 2013; Gilmore, Savell and Collin, 2011) A review of literature (not authored or sponsored by industry) found no evidence to support effectiveness or safety of food industry self-regulation or public-private partnerships with “highly processed” food industry
to improve public health (Moodie et al., 2013; Lewin et al, 2006) Most research cautions against working with the “highly processed” food industry for the purpose of public health for several reasons. Although industries strongly assert that self-regulation is sufficient to protect the public, there is no enforcement of third party monitoring of their effects (Lewin et al, 2006) and researchers assert that they may be self-serving, stall other potential government action, and protect “business as usual” (Moodie et al., 2013; Sharma, Teret and Brownell, 2010; Brownell & Warner, 2009) Similarly, companies have modified product formulas and promised to shift marketing efforts toward more nutritious products, while continuing to make and promote less nutritious versions (Moodie et al., 2013; Lewin et al, 2006) Following their review of processed food company promises versus practice, Lewin and colleagues (2006) state that for business reasons alone, these companies cannot –
and will not – stop making and marketing nutritionally questionable food products to children. Sharma and colleagues state that food industry self-regulation may only succeed “with public health input in the planning and execution of regulations, transparency in creating standards, and external, objective evaluation of impact” (Sharma et al, 2010). 7 There is an inherent conflict of interest between public health goals and that of “highly processed” food industry due their legal responsibility to make a profit to return to investors (Wiist, 2011). More specifically, some stipulate that the highly processed food industry has two basic strategic options to enhance shareholder revenue: 1) persuade consumers to eat more; or 2) increase profit margins, especially by marketing reformulated or repackaged products (Ludwig & Nestle, 2008). And since much higher profits come from processed foods compared to fresh foods, advising people to eat less or more healthily contradicts
the core business models of food companies (Ludwig & Nestle, 2008). There are other, less obvious risks to partnering with “highly processed” food industry. Literature states that food industry often uses similar tactics as tobacco to build relationships with public health organizations by promising to self-regulate and/or funding public health initiatives in order to gain influence at the public health table and undermine more effective public health action that would affect their bottom line (Moodie et al., 2013; Gilmore et al, 2011; Koplan & Brownell, 2010; Brownell & Warner, 2009; Ludwig & Nestle, 2008; Lexchin, Bero, Djulbegovic, & Clark, 2003). “Most researchers caution public health professionals and organizations to be aware that corporate enticements of partnerships and funding can blur or disguise the distinction between these differing purposes, goals and values .” Studies also suggest that food industry has an “especially insidious
influence” on the conduct of research and development of public health policy (Ludwig & Nestle, 2008) and challenging the integrity of research that challenges their bottom line (Moodie et al., 2013; Tereskerz, Hamric, Uterbock, & Moreno, 2009; Gilmore et al, 2011) Overall, there is a risk of perceived loss of integrity of a public health organization when associated with “highly processed” food industry who market products that directly conflict with public health recommendations (e.g high in fat, sugar, sodium). Food companies often pressure health organizations to enter cause-related marketing relationships, offering the appeal of leveraging these companies’ broad reach to public health organizations with limited resources. The results may undermine the credibility of these public health organizations and may facilitate access to companies to enhance the marketing of energy-dense products by association with trusted health organizations (Kraak, Kumanyika & Story,
2009). Research warns when favourable nutrition information and/or health claims are presented on products, consumers have more favourable attitudes, including nutrition attitudes, and purchase intentions towards the product (Kozup, Kreyer & Burton, 2003). Furthermore, some have questioned whether industry should be entrusted to convey public health messages by using advertising as a solution to address a problem attributed to excessive advertising (Schor & Ford, 2007). 8 Although research shows that exclusive focus on physical activity is insufficient to offset excess energy consumption associated with marketing practices that promote unhealthy diets (Ludwig & Nestle, 2008) it is increasingly common for “highly processed” food industry to deflect negative attention from processed foods and sugar-sweetened beverages by focusing resources and marketing on physical activity, “implicitly de-emphasizing the role of food quality and portion size in reducing obesity
risk” and placing sole responsibility on the individual (Kraak, Kumanyika, & Story, 2009; Lewin et al., 2006; Koplan & Brownell, 2010). Some literature therefore cautions against cobranding with these companies in an effort to eliminate contradictions in both explicit and implicit healthy lifestyle messages children receive around food and activity choice (Hesketh, Waters, Green, Salmon & Williams, 2005). Intrinsically, the purpose, goal and values of public health and that of processed food corporations are fundamentally different. Most researchers caution public health professionals and organizations to be aware that corporate enticements of partnerships and funding can blur or disguise the distinction between these differing purposes, goals and values (Moodie et al., 2013; Wiist, 2011; Ludwig & Nestle, 2008; Brownell & Warner, 2009). Of further concern is that at the end of the day, “when public health and corporate goals conflict, corporate profit
imperatives often trump public health imperatives” (Lewin et al., 2006) 9 Benefits Experiences Across Canada A survey was conducted to capture experiences, interests and challenges faced across Canada in developing PPPs with the food industry. According to the survey, retailers represented by grocery stores, convenience stores and farmers’ markets seem to be “the most popular” food sector to engage with. Partnerships seem most likely to happen with retailers, often to promote healthy food at point-ofpurchase, followed closely by growers (e.g fruit and vegetables) and producers (eg milk, eggs). Most jurisdictions who responded to the survey indicated that they were interested in developing a national framework and/or sharing information, knowledge and expertise on PPPs with the food industry. For example, one jurisdiction mentioned that the “food industry is multi-national and affects most Canadian jurisdictions” and that by working together, we would have “stronger
influence”. A national dialogue on how to engage with the food industry will allow jurisdictions to capitalize on the expertise and knowledge of other jurisdictions and provide guidance to help governments address the challenges and risks involved in public-private partnerships. See Appendix 1 for more detail. 10 The food industry has made some voluntary attempts to introduce or reformulate existing products to promote healthier choices (Swinburn, Sacks & Hall, 2011; Gortmaker, Swinburn & Levy, 2011; WHO, 2004). The primary motivation might not be to promote better nutrition or to reduce dietary risks. It may simply reflect the recognition that nutrition and dietary issues will continue to be of concern to many governments, researchers, international organizations, professional organizations, advocacy groups and consumers (Cash, 2006; Popkin, 2009). For example, PepsiCo through its subsidiary Frito-Lay has eliminated trans-fats from its salty snacks and developed some
baked-snack options (Cash, 2006). Danone, a global producer of bottled water products, has reduced the sugar content in its sweetened water by 40 percent (compared to its original calorie value) in six countries. Others companies, such as Kraft, Nestle, Unilever have also worked on reducing calories and added sugar in many of their products (Popkin, 2009). In Canada, Loblaw’s introduced the PC Blue Menu Line with the aim of making healthier eating easy and affordable. This line now contains more than 400 products with at least one of the following health benefits: lower fat, lower calories, high fibre, omega-3, soy protein, and lower sodium (Loblaws, 2008). Despite the importance of these measures, the food industry is not eliminating the “unhealthy” food products of their line to truly alter dietary behaviours at a population level (Popkin, 2009). Although it is still not known whether these voluntary measures will promote health benefits at a population level, the reformulation
of these products have resulted in healthier choices (e.g less sugar or less sodium) (De Pinho, 2012). Until recently, the role of the private sector in public health has been viewed with “antagonism, suspicion, confrontation” (Lucas, 2002) by many actors in the field. Governments and inter-governmental organizations are now recognizing that it is necessary to involve multiple stakeholders, including the private sector in the pursuit of a healthy and sustainable society (Rowitz, 2006; WHO, 2004). This recognition has been accompanied with a reassessment of the roles, strengths and limitations of the public sector, the private sector and the civil society in responding to health problems (Widdus, 2001). Proponents of PPPs for public health argue that this form of collaboration has become compelling in an environment of complex health problems (Widdus, 2001), tremendous community need and competition for limited resources (Reich et al, 2003). This is an environment in which neither
side can on its own achieve its specific goals (Lucas, 2002). According to Widdus, partnerships seem to be most justifiable when traditional ways of working independently have a limited impact on a problem, the specific desired goals can be agreed by the collaborating players, complementary expertise is interchanged between both sectors, the long-term interests of each sector are fulfilled (i.e there are benefits to all players involved) and contributions of expertise and resources are reasonably balanced (Widdus, 2001). Whether strategies for obesity prevention are based on increasing physical activity or promoting healthy eating or on both, the strategies cannot be seen as the sole responsibility of one sector (WHO, 2000). The Lancet’s series on obesity prevention suggests that the obesity epidemic is driven by complex forces that require a systems approach to reverse the obese epidemic, further suggesting that strategies be multisectoral and involve the active participation of
governments and the food industry (Gortmaker et al, 2011; WHO, 2000). Governments are important actors in reversing the obesity epidemic, because protection and promotion of public health is a core responsibility of government (Gortmaker et al, 2011). The food industry is also a significant player due to its role in producing, distributing and providing food products Governments around the world have allocated this role to the private sector and allowed companies to generate economic activity from food, which is a product essential for public life and health (Hawkes and Buse, 2011). The Global Strategy on Diet, Physical Activity and Health by the WHO suggests that the private sector become partners with governments to facilitate and enable integrated efforts to encourage healthier environments (WHO, 2004). The shared responsibilities and partnerships between the public and private sector allows for multiple strategies for the prevention and management of obesity (WHO, 2000) and
multifaceted solutions that cut across sectors (Gortmaker et al 2011). To reduce obesogenic environments, which is defined as “the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations” (Lake, 2006: 262), a multi-sectoral approach that mobilizes the combined energy, resources and expertise of all actors is essential for sustained progress. This collective power can achieve sustainable change (Gortmaker et al, 2011; WHO 2003) in a number of core activity areas, including: 1. Health Promotion and communication campaigns (e.g information leaflets and posters); 2. Diet and nutrition education in formal and informal leaning venues (e.g building cooking skills); 3. Communicating information on food products (eg nutrition labeling and healthy food logos); 4. Controlling advertising and marketing of food products (eg advertising codes on marketing); 5. Increasing or decreasing access to food products (eg
fruits and vegetables, vending machines); 6. Conducting or supporting research (eg on development of novel foods); 7. Developing or reformulating food products (eg reducing sodium); 8. Developing recommendations, guidelines, advice, and strategies for governments and industry (e.g government forum that includes the food industry); 9. Encouraging private sector action in general, such as providing a forum for commitments (eg platforms); and, 10. Funding for above activities connected to healthy eating (Hawkes and Buse, 2001: 7). Some scholars claim that PPPs can bring meaningful social changes in the promotion of physical activity and healthful eating (Kraak & Story, 2010). In their view, PPPs should prioritize policies with a broader population-based approach rather than those policies focused on individual behavioural approaches. Other scholars go further in claiming that if properly designed, PPPs for obesity prevention can expedite the adoption of new rules that apply to a wide
range of competing companies (Huang & Yaroch, 2009). If well developed, PPPs with the food industry may offer several advantages for governments to make progress in these areas and provide other benefits (De Pinho, 2012), such as: Better understanding of each other; Collaborative rather than confrontational approach (food industry might be willing to comply with government’s interventions); Innovative mechanism to address societal problem; Leverage food industry expertise; Leverage food industry resources; Provide access to industry data, information, and expertise for research and evaluation (e.g sales data); and Influence food industry practice towards healthy eating. 11 Key Considerations Due to the broad spectrum of potential partners for PPPs to increase public health, it is important to acknowledge that PPPs involve different types of engagement and activities (Hawkes & Buse, 2011). This is especially evident when referring to food
industry given the diversity of segments (i.e, manufactures, producers, retailers, restaurant services) For example, an engagement with food retailers on health messaging is very different from a research collaboration or a forum for discussing reducing marketing to children with manufacturers. No clear guidelines and governance structures exist to guide public health organizations’ decisions on whether and how to engage effectively and efficiently with the food industry (Hawkes & Buse, 2011). A comprehensive but flexible tool is needed in order to: 1) Determine whether private sector engagement would help advance the public health goals and, if so, set criteria for private sector engagement; 2) Define the type of engagement activity; 3) Identify shared goals and possible conflicts of interest; 4) Assess the influence of potential private partners on public health research and policy; and 5) Establish a good governance structure. First, it is important to set criteria for private
sector engagement. Some claim that the current reality is one where public-private collaborations have assumed a role in the exercise of power that affect decisions about how to address chronic diseases and their modifiable factors, like healthy eating (Hawkes & Buse, 2011). In order to ensure that partnerships will advance public health goals and avoid conflict or interest or lost integrity, academics and some in the public health field are calling for clear guidelines to assist organizations to clarify the purpose, terms and management of private-sector engagement. In the context of healthy eating, Hawkes (2011) urges that “it is only after the public health objective has been set that policy makers should even think about engaging with the food industry”. This does not mean there can be no engagement, but Hawkes (2011) suggests only doing so after answering these three questions: 1. Would engaging with food industry help achieve the objective faster and more effectively? 2.
Would the interests involved (on both sides) enhance or threaten the likelihood of achieving the specific objective as well as longer-term public health objectives? 3. If interaction is a viable option, what form of engagement would most effectively achieve the objective while accounting for the different interests: a real partnership or less formal type of collaboration? It is crucial that the partnership or collaboration only be initiated if it will help advance the public health goal, and that the partnership itself it not seen as the outcome (Nishtar, 2004). With the public health goal paramount, not partnering or disengaging is always an option, and sometimes the better one, since “incompatible and poorly executed partnerships can damage public trust, credibility and all partners’ brand reputations” (Kraak et al., 2011) along with potentially causing more harm to public health than not undertaking the initiative in the first place (Brady & Rundall, 2011; Hawkes &
Buse, 2011; Brownell, 2012). 12 Second, it is important to distinguish between a partnership and the broader term of ‘collaboration’, and whether there is a responsible way to engage with the food industry. Some experts believe that collaboration may work if strict criteria are established and a risk analysis is conducted at the outset, transparency and accountability mechanisms are firmly established, and any decision to collaborate is based solely on the ultimate public health objective (Kraak et al., 2009) The term Info graphic: Who owns what in the food industry? (Source: Fritz Kreiss/Occupy Monsanto) “partnership” in the literature refers to anything from education campaigns to joint research activities and may involve a range of processes and structures. But as Hawkes writes: There is an important distinction that can be made: interactions characterized by ‘shared decision-making power among partners’ and those characterized simply by ‘participation’ from
both sectors. In the former, both sectors play a role in decisions about the agenda, goals, strategies, resources, roles and responsibilities of the initiative; in the latter, there may be mutual support, but no shared decision-making. The distinction between ‘partnership’-based and ‘participation’-based initiatives may appear academic and even immaterial given that influence in decision-making can be exerted in the absence of formal structures for decision-making. Still, making the distinction is critical. For a start, using the term ‘partnership’ imprecisely can create misleading expectations For example, a public sector-led initiative may embrace private sector actors as ‘partners’ even when its only interest is gaining private sector concessions or funding with few or no conditions. But by giving the impression to the private sector that it is a real ‘partner’, the public sector is, like it or not, inviting for-profit actors to use the arrangement to serve their
own private sector interests If public health officials want to draw on the potential power of civil society to serve their interests, they would be advised to be clearer about when they need civil society ‘participation’ in an initiative, or actual ‘partners’ (Hawkes and Buse, 2011: 400-01). It is crucial to distinguish the type of engagement a public health organization aims to enter with industry. For example, ‘partnership’ is appropriate when the interaction involves both sectors having a voice in decision-making. If decision making is not shared, terms like ‘interaction’ or ‘engagement’ should be used in order to be clear (Hawkes & Buse, 2011) Third, researchers have identified shared goals and possible conflicts of interest as an imperative consideration when engaging in PPPs. The key to the effectiveness of these relationships is the avoidance of conflict of interest (Kraak et al 2011; Kraak and Story, 2010). If the public health goals and those of the
industry collaborator do not conflict, there is potential for an effective collaboration Avoiding conflict of interest is challenging when choosing food industry collaborators to prevent obesity or promote healthy eating due to inherent business objectives of some segments of the industry (Wiist, 2011; Gilmore et al., 2011) However, the concept of shared goals and working with other private sector collaborators with whom there is no potential conflict of interest could hold promise 13 Fourth, governments need to consider the influence of the private sector over research and public health policy. Lesser et al (2007) analyzed 206 nutrition-related scientific articles published over a 5-year period that addressed the health effects of milk, fruit, juices, and soft drinks. The likelihood of a conclusion favourable to the financial interests of the sponsoring company was 4fold to 8-fold higher if the study received full rather than no industry funding, pointing to a systematic bias.
Food companies also donate large sums of money to professional associations in order to receive “a national platform via events and programs with prominent access to key influencers, thought leaders and decision makers” (Ludwig and Nestle, 2008) in an attempt to “gain a seat” at in those forums and influence public health policy (Moodie et al., 2013; Lexchin et al, 2003; Gilmore et al, 2011; Koplan & Brownell, 2010) For example, 10 of 12 partners and sponsors of the American Academy of Nutrition and Dietetics are processed food companies (Academy of Nutrition and Dietetics’ website, 2013). In a recent report, public health attorney and author Michele Simon claimed that this undermines the integrity of those professionals most responsible for educating Americans about healthy eating (Simon, 2013). Throughout the literature, there is considerable evidence that companies use tactics to undermine public health taxation and regulations (Stuckler and Nestle, 2012) and deflect
criticisms of their core practices by introducing and promoting healthier processed foods (Brownell, 2012 and Moodie et al, 2013). “A well designed and executed partnership can support transformative systems change while an incompatible and poorly executed one can damage public trust and the credibility of all partners.” Lastly, to maximize benefits and minimize risks, good governance structures are required to support government collaboration with the food industry. There is a governance gap and no clear structure in place to enable governments to engage with the food industry to promote healthy eating (Hawkes and Buse, 2011). This makes it important to establish formal governance structures when collaborating with private partners. The type of engagement and kind of activity to be undertaken must be considered as different skills, functions, resources, roles and responsibilities are required. Any identified risks should also be addressed within the governance structure as it is
designed (Hawkes and Buse, 2011). Accountability processes should be developed within the governance structure to balance private and public health interests, manage conflicts of interest, ensure co-branded activities support healthy products and healthy eating environments, comply with ethical codes of conduct, assess partnership compatibility and monitor partnership outcomes (Kraak et al, 2011). Given the risks involved for both public and private partners, a process to disengage and dissolve a partnership should be established within the governance structure. A well designed and executed partnership can support transformative systems change while an incompatible and poorly executed one can damage public trust and the credibility of all partners (Kraak et al, 2011). 14 Conclusion Encountering challenges is inherent to the process of deciding whether to develop PPPs with the food industry. In order to overcome these challenges, governments need to consider a number of issues
before pursuing engagement opportunities. It is important to be clear on underlying goals of potential partners and determine whether: 1) collaboration will advance short and long-term public health goals, 2) what type of engagement activity is most effective (e.g platform for discussion, alliance, partnership), and 3) the goals of the potential collaborator are not in conflict with the public health objective. A number of jurisdictions across Canada are already engaged in PPPs with food industry and have expressed interest in a national dialogue on this issue. This paper will support that dialogue and is the first step in developing a national framework on how to engage with the food industry. 15 Appendix 1: Interest and Experience across Canada In addition to completing a literature review, a brief survey was conducted to capture experiences, interests and challenges faced across Canada in developing PPPs with the food industry. In November 2012, the Public Health Agency of
Canada circulated the survey to all 13 provinces and territories. Eight out of 13 jurisdictions responded the survey. Six jurisdictions reported that they have engaged with the food industry and seven reported that they are very interested or interested in exploring options for partnerships with the food industry. Among the six jurisdictions that have engaged with the food industry, all of them have entered into a partnership model, and more than half have engaged in a “platform for discussion” created for information sharing. The majority of jurisdictions have also engaged in lower levels of engagement through donation or sponsorship Jurisdictions have reported multiple types of engagement with the food industry and are approaching the full spectrum of the food sector ranging from producers to retailers. According to the survey, retailers represented by grocery stores, convenience stores and farmers’ markets seem to be “the most popular” food sector to engage with.
Partnerships seem most likely to happen with retailers, often to promote healthy food at point-of-purchase, followed closely by growers (e.g fruit and vegetables) and producers (e.g milk, eggs) Each jurisdiction was asked to rank which type of partnership would be most relevant to their jurisdiction. Partnerships to increase access to healthy foods (eg fruit and vegetables) were viewed as the most relevant type of partnership to develop with the food industry, followed by partnerships for public education and information (e.g promotion of healthy-eating messages, food skills, etc) These two types of partnerships do not seem to be mutually exclusive, as public education and information approaches can be used to promote access to healthy foods. In any partnership, partners expect to obtain certain benefits as the result of the engagement. It was interesting that jurisdictions across Canada expect, as the most important benefit, to influence food industry practices to promote healthy
eating while leveraging food industry resources (e.g financial, human and physical resources) and their ability to “get the message out” efficiently Jurisdictions also acknowledged that the most appropriate role for the government in a PPP with the food industry is to build trust among partner organizations and provide leadership in the overall partnership. These aspects are also reported in other examples of PPPs for public health (e.g PPPs with pharmaceutical companies, partnerships with private health providers). Research indicates that there is still considerable skepticism about the motives of the private sector in partnering with the public sector. This skepticism can undermine any attempt to overcome mistrust among partner organizations and create an environment for collaboration. Building trust among partner organization is an essential step in the process of developing a PPP (De Pinho, 2012). The question is how to make the most of the food industry’s role and expertise
to prevent obesity presents numerous challenges. Conflicting values (often explained by the profit motives vs. public health goals) and the perceived co-option of publichealth goals by commercial interest were identified by jurisdictions as the most risky aspects of engaging with the food industry. Scholars have suggested that partner organizations adopt systematic and transparent accountability processes in order to maximize the benefits and reduce these types of risks. For example: 16 Managing conflict of interest and bias in decision making; Ensuring that co-branded activities support healthy products and healthy eating; Complying with ethical codes of conduct; Undertaking due diligence to assess partnerships; and, Monitoring and evaluating partnership outcomes. Government priorities seem to determine whether a jurisdiction decides to enter into a partnership with the food industry, followed by having a previous or existing relationship with the food
industry. Jurisdictions that had not engaged with the food industry provided reasons related to conflicting values/goals between the public and the privates sectors, concerns about public perception and limited organizational capacity to build these partnerships. Jurisdictions with previous experience in engaging with the food industry reported similar challenges (e.g mistrust of industries to partner with the government; different priorities among partner organizations, etc.) Other challenges included: finding an appropriate partner for effective partnerships; the need for a champion to facilitate access to industry partners; appropriate measures for monitoring the purchase and consumption of healthy food; the need to ‘recognize’ the efforts and achievements of the food industry; and, the need to ensure program sustainability. At the same time, jurisdictions reported positive outcomes, such as: Increased awareness and demand for local foods by establishing venues for
dialogue with consumers about topics associated with food (e.g food preparation); Interest from the food and beverage industry in supporting healthy eating programs such as school healthy eating policies; and Increased availability and accessibility to foods such as fruit and vegetables by increasing investments in local food infrastructure and partnership development with the food industry and promotion of healthy food at pointof-purchase. Jurisdictions also reported a number of lessons learned, such as: Making initiatives voluntary but “irresistible”; Maximizing linkages with other partners and programs; Maintaining communication is essential; and Having leadership at the federal level is required to support consistent messaging regarding healthy eating and PPPs. Most jurisdictions who responded to the survey indicated that they were interested in developing a national framework and/or sharing information, knowledge and expertise on PPPs with the food industry.
For example, one jurisdiction mentioned that the “food industry is multi-national and affects most Canadian jurisdictions” and that by working together, we would have “stronger influence”. A national dialogue on how to engage with the food industry will allow jurisdictions to capitalize on the expertise and knowledge of other jurisdictions and provide guidance to help governments address the challenges and risks involved in public-private partnerships. 17 Reference List Academy of Nutrition and Dietetics. Who are the Academy’s Corporate Sponsors: http://wwweatrightorg/ corporatesponsors/ (retrieved March 2013). Agurto I, Rodriguez L, Zacarias I. (2011) Food and vegetable promotion and the 5-a-day programme in Chile for the prevention of chronic non-communicable diseases: across-sector relationships and public-private partnerships. In: Blas E, Sommerfeld J, Sivasankara Kurup A (eds.) Social Determinants Approaches to Public Health: from concept to practice World Health
Organization: Geneva 2011 Asante AD, Zwi AB. (2007) Public-private partnerships and global health equity: prospects and challenges Indian Journal of Medical Ethics, 4, 176-80 Balasubramanian R, Rajeswari R, Vijayabhaskara RD, Jaggarajamma K, Gopi PG, Chandrasekaran V, et al. (2006) A rural public-private partnership model in tuberculosis control in South India. International Journal of Tuberculosis and Lung Disease, 10, 1380-85. Boyle DP, Gardner J, Callaway J. (1998) A partial hospitalization program provided through a public-private partnership Clinical gerontologist, 19, 21-37 Brady, M., & Rundall, P Governments should govern, and corporations should follow the rules SCN News 2011, 39, 51 -56. Bravo NR. (2007)The challenge for NIH ethics policies: preserving public trust and biomedical progress Cleveland Clinic journal of medicine, 74, S29-31 Brownell, K.D, Kersh, R, Ludwig, DS, Post, RC, Puhl, RM, Schwartz, MB & Willett, WC (2010) Personal Responsibility and Obesity: A
Constructive Approach to a Controversial Issue Health Affairs, 29(3), 379-387 Brownell, K.D, & Warner, KE (2009) The Perils of Ignoring History: Big Tobacco Played Dirty and Millions Died How Similar is Big Food? The Milbank Quarterly, 87(1), 259-294. Brownell, K.D (2012) Thinking forward: The quicksand of appeasing the food industry PLoS, 9(7), e10001254 Buse K, Walt G. (2000) Global public-private partnerships: part II - what are the health issues for global governance? Bulletin of the World Health Organization, 78, 699-709. Buse K, Waxman A. (2001) Public-private health partnerships: a strategy for WHO Bulletin of the World Health Organization, 79, 748-54 Cash SB, Goddard EW, Lerohl M. (2006) Canadian Health and Food: The links between Policy, Consumers and Industry Canadian Journal of Agricultural Economics, 54, 605-29. Clasen TF. (2002) The public-private partnership for the Central American hand washing initiative: reflections from a private sector perspective. Tropical
Medicine & International Health, 7, 197-200 De Pinho Campos, K. (2012) Public-Private Partnerships for Obesity Prevention Paper prepared for the qualifying examination of the doctoral program in the Dalla Lana School of Public Health, University of Toronto (unpublished) De Pinho Campos , K., Norman, CD, Jadad, AR (2011) Product development public-private partnerships for public health: A systematic review using qualitative data. Social science & medicine, 73, 986-94 Dewan, P.K, Lal, SS, Lonnroth, K, Wares, F, Uplekar, M, & Sahu, S, et al (2006) Improving tuberculosis control through public-private collaboration in India: literature review. BMJ, 332, 574-78 Field JE, Peck E. (2003) Public-private partnerships in healthcare: the managers perspective Health & Social Care in the Community, 11, 494-501. Gilmore, A.B, Savell, E, & Collin, J (2011) Editorial: Public health, corporations and the new responsibility deal: promoting partnerships with vectors of disease?
Journal of Public Health 33(1), 2-4 18 Gortmaker, S.L, Swinburn, BA, Levy, D, Carter, R, Mabry, PL, Finegood, DT, Huang, T, March, T, & Moodie, M (2011). Changing the future of obesity: science, policy, and action Lancet,378, 838-847 Hardon A. (2006) Immunisation for all?: A critical look at the first GAVI partners meeting HAI Europe, 6 (1), 2-9 Hawkes, C. (2004) Marketing Food to Children: the Global Regulatory Environment Geneva: World Health Organization; http://whqlibdoc.whoint/publications/zoo4/9241I591579pdf (Retrieved March 2013) Hawkes C. (2008) Working Paper on Public-Private Partnerships for Health High Level Group - Working Paper European Commission 2008. Hawkes C, Buse K. (2011) Public health sector and food industry interaction: its time to clarify the term partnership‚ and be honest about underlying interests. The European Journal of Public Health, 21, 400-01 Hawkes C, Buse K. Public-Private Engagement For Diet and Health: Addressing the Governance Gap SCN News
2011; 39: 6-10. Hesketh, K., Waters, E, Green, J, Salmon, L, & Williams, J (2005) Healthy eating, activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion International, 20(1), 19-26 Huang TT, Yaroch AL. (2009) A public-private partnership model for obesity prevention Preventing Chronic Disease, 6 (3), 1-2. Huxham C, Vangen S, Huxham C, Eden C. (2000) The Challenge of Collaborative Governance Public Management Review, 2, 337-57 Kickbusch I, Lister G. (2006) Europe must establish a societal dialogue for global health: Public-private partnership European Perspective on Global Health: A policy glossary European Foundation Centre: Brussels, Belgium 2006 Koplan, J.P, & Brownell, KD (2010) Response of the Food and Beverage Industry to the Obesity Threat JAMA 304(13), 1487-1488. Kozup, J.C, Kreyer, E H, & Burton, S (2003) Making Healthful Food Choices: The Influence of Health Claims and Nutrition Information on Consumers
Evaluations of Packaged Food Products and Restaurant Menu Items Journal of Marketing 67(2), 19-34 Kraak VI, Kumanyika SK, Story M. (2009) The commercial marketing of healthy lifestyles to address the global child and adolescent obesity pandemic: prospects, pitfalls and priorities. Public Health Nutrition, 2009, 12, 2027-36 Kraak VI, Story M. (2010) A public health perspective on healthy lifestyles and public-private partnerships for global childhood obesity prevention. Journal of the American Dietetic Association, 110, 192-200 Kraak VI, Swinburn BA, Lawrence JM, Harrison P. (2011) The Accountability of Public-Private Partnership with Food, Beverage and Quick-Serve Restaurant Companies to Address Global, Hunger, and the Double Burden of Malnutrition. SCN News, 39, 11-22. Lake, A. (2006) Obesogenic environments: exploring the built and food environments The Journal of The Royal Society for the Promotion of Health, 126(6), 262-267. Lesser, L.I, Ebbeling, CB, Goozner, M, Wypij, D, &
Ludwig, DS (2007) Relationship between funding source and conclusion among nutrition-related scientific articles PLoS Med, 4(1), e5 Levine OS, Cherian T, Shah R, Batson A. (2004) PneumoADIP: An example of translational research to accelerate pneumococcal vaccination in developing countries Journal of Health, Population and Nutrition, 22, 268-74 Lewin A, Lindstrom L, Nestle M. (2006) Food Industry Promises to Address Childhood Obesity: Preliminary Evaluation Journal of Public Health Policy, 27, 327-454. Lexchin, J., Bero, LA, Djulbegovic, B, & Clark, O (2003) Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ, 326, 1160-1170 Loblaw. (2008) The Way We Do Business Corporate Social Responsibility Report Loblaw Companies Limited 19 Lonnroth K, Uplekar M, Arora VK, Juvekar S, Lan NTN, Mwaniki D, et al. (2004) Public-private mix for DOTS implementation: what makes it work? Bulletin of the World Health Organization, 82, 580-86 Lucas AO.
Public-Private Partnerships: Ilustrative Examples In: Reich MR (ed) (2002) Public-Private Partnerships for Public Health. Harvard University Press: Cambridge, MA 2002 Ludwig, D.S, & Nestle, M (2008) Can the Food Industry play a constructive role in the obesity epidemic? J am Med Assoc, 300, 1808-1811. Meredith S, Ziemba E. (2007) A new landscape of partnerships Global Forum Update on Research for Health: Equitable Access: Research challenges for health in developing countries Global Forum for Health Research: Geneva, Switzerland 2007 Ministry of Health of Canada. Sodium Reduction Strategy for Canada: Recommendations of the Sodium Working Group. In: Division NE (ed) Ministry of Health of Canada: Ottawa 2010 Mitchell-Weaver C, Manning B. (1991) Public-private partnerships in third world development: A conceptual overview Studies in Comparative International Development (SCID), 26, 45-67 Moodie, R., Stuckler, D, Monteiro, C, Sheron, N, Neal, B, Thamarangsi, T, Lincoln, P, &
Casswell, S (2013) Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. The Lancet, 381(9867), 670–679. http://dxdoiorg/101016/S0140-6736(12)62089-3 (retrieved March 2013) Newell JN, Pande SB, Baral SC, Bam DS, Malla P. (2005) Leadership, management and technical lessons learnt from a successful public-private partnership for TB control in Nepal. International Journal of Tuberculosis and Lung Disease, 9, 1013-17. Nishtar S. (2004) Public-private partnerships in health - A global call to action Health Research Policy and Systems, 2 (5), 1-7. Patouillard E, Goodman CA, Hanson KG, Mills AJ. (2007) Can working with the private for-profit sector improve utilization of quality health services by the poor? A systematic review of the literature International Journal for Equity in Health, 6, 6-17. Peters BG. (1998) With a Little Help From Our Friends: Public-Private Partnerships as Institutions and Instruments In: Pierre J
(ed.) Partnerships in urban governance : European and American experience St Martins Press Inc: New York 1998; 11-33. Popkin BM. (2009) The World Is Fat: The fads, trends, policies, and products that are fattening the human race New York: Penguin Group (USA). Reich, M. R (2000) Public-private partnerships for public health Nature medicine, 6: 617-20 Reich MR. (2002) Public-private partnerships for public health Cambridge, MA: Harvard University Press Reich MR, Hershey JH, Hardy GE, Jr., Childress JF, Bernheim RG (2003) Workshop on public health law and ethics I & II: The challenge of public/private partnerships (PPPs). Journal of Law, Medicine & Ethics, 31 (s4): 90-93 Richter, J. (2004) Public-Private Partnerships for Health: A Trend with no alternatives? Development, 47: 43-48 Ridley RG. (2001) Putting the "partnership" into public-private partnerships WHO Drug Information, 15, 57-58 Rowitz L. (2006) Public Health for the 21st Century: the prepared leader Sudbury,
MA: Jones and Bartlett Publishers, Inc. Schor, J. & Ford, M (2007) From tastes great to cool: children’s food marketing and the rise of the symbolic J Law Med Ethics 35, 10–21. Sharma, L.L, Teret, SP, & Brownell, KD (2010) The Food Industry and Self-Regulation: Standards to Promote Success and to Avoid Public Health Failures. American Journal of Public Health, 100(2), 240-246 20 Simon, M. (2013) Are America’s nutrition professionals in the pocket of Big Food? Eat Drink Politics: http:// www.appetiteforprofitcom/2013/01/22/and-now-a-word-from-our-sponsors-new-report-from-eat-drink-politics/ (retrieved March 2013). Stuckler D, Nestle M. (2012) Big Food, Food Systems, and Global Health PLoS Med 9(6): e1001242 doi:101371/ journal.pmed1001242 Swinson, B.A, Sacks, G, Hall, KD, McPherson, K, Finegood, DT, Moodie, ML, & Gortmaker, SL (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet, 378, 804-814 Tereskerz, P., Hamric, AB,
Uterbock, TM, & Moreno, JD (2009) Prevalence of industry support and its relationship to research integrity. Accountability in Research, 16, 78–105 The Canadian Council for Public-Private Partnerships. Definitions of PPP Toronto 2011; http://wwwpppcouncilca/ resources/about-ppp/definitions.html The Pharmaceutical Security Institute. Partnership for Safe Medicines http://wwwsafemedicinesorg/: 2011 Van Huijstee MM, Francken M, Leroy P. (2007) Partnerships for sustainable development: a review of current literature Environmental Sciences, 4, 75-89 WHO. (2000) Obesity: Preventing and Managing the Global Epidemic, Technical Report Series No 894 Geneva: World Health Organization: http://whqlibdoc.whoint/trs/WHO TRS 894pdf, (retrieved March 2013) WHO. (2002) Health: Marketing and Youth Conference Italy: World Health Organization: http://wwwwhoint/healthmktg/ about conferencehtm (retrieved March 2013) WHO (2003). FAO Diet, Nutrition and the Prevention of Chronic Diseases, Technical
Report Series No 916 Geneva: World Health Organization: http://whqlibdoc.whoint/trs/WHO TRS 9 6pdf (retrieved March 2013) WHO (2004). Global Strategy on Diet, Physical Activity and Health Retrieved from http://wwwwhoint/ dietphysicalactivity/strategy/eb11344/strategy english web.pdf Widdus R.(2005) Public-private partnerships: an overview Transactions of the Royal Society of Tropical Medicine & Hygiene, 99, S1-8 Widdus R. (2001) Public-private partnerships for health: their main targets, their diversity, and their future directions Bulletin of the World Health Organization, 79, 713-20. Wiist, B. (2011) The Risks to Public Health from Partnerships with Corporations Corporations and Health Watch: Tracking the effects of corporate partnerships on health http://corporationsandhealthorg/2011/05/11/the-risks-to-publichealth-from-partnerships-with-corporations/ (retrieved March 2013) Yerby MS. (1998) A north american registry for epilepsy and pregnancy, a unique public/private partnership
of health surveillance. Epilepsia, 39, 793-98 21 Multi-Sectoral Partnership Task Group The mandate of the Task Group is to develop a guiding framework to support jurisdictions to undertake an evidence-informed approach to partnership development with the food industry. This Task Group will be established from March to September 2013 The goals of the Task Group are to: Articulate how PPPs from public health differ from other types of engagements with the private sector; Explore how PPPs for public health are organized and their objectives; Identify key issues when assessing the development of partnerships between the government and the food industry; Discuss mechanisms/tools for the partnership development with the food industry; and Provide examples of empirical PPPs in diet, nutrition and obesity prevention nationally and internationally. 22